Medications for Opioid Use Disorder

- Prevent and Manage Opioid Misuse – Educate others, promote safe practices, and encourage access to effective treatments.
- Ensure Safety – Take opioids only as prescribed, store them securely, and properly dispose of unused medications.
- Manage Pain Responsibly – Work with your healthcare provider to explore safe, non-opioid pain management alternatives.
- Understand Addiction – Recognize addiction as a chronic disease; with the right treatment, recovery is possible.
- Be Prepared – Keep naloxone, an opioid overdose reversing drug, on hand and know how to use it to save lives during an opioid overdose.
Opioid Use Disorder (OUD) is a chronic, treatable medical condition, with diagnoses and opioid misuse rising dramatically in recent years. Misuse includes taking opioids beyond prescribed amounts or using them in ways like snorting or injecting to enhance effects. Many individuals with OUD or misuse obtain opioids from prescriptions or from friends and family, leading to both intentional and accidental overdoses.
IHS focuses on ensuring comprehensive, culturally appropriate care for those with OUD. Through Medications for Opioid Use Disorder (MOUD), IHS integrates evidence-based treatments—combining pharmacological interventions with counseling and culturally supportive services. MOUD has been shown to reduce withdrawal symptoms, cravings, illicit use, and overdose risk, while improving treatment retention and survival.
To enhance access to MOUD, IHS implemented Special General Memorandum 19-01, requiring all federal facilities to identify local OUD resources and create action plans by December 11, 2019, to expand access to culturally sensitive prevention, treatment, and recovery services.
Managing OUD
Engagement at any step in the journey
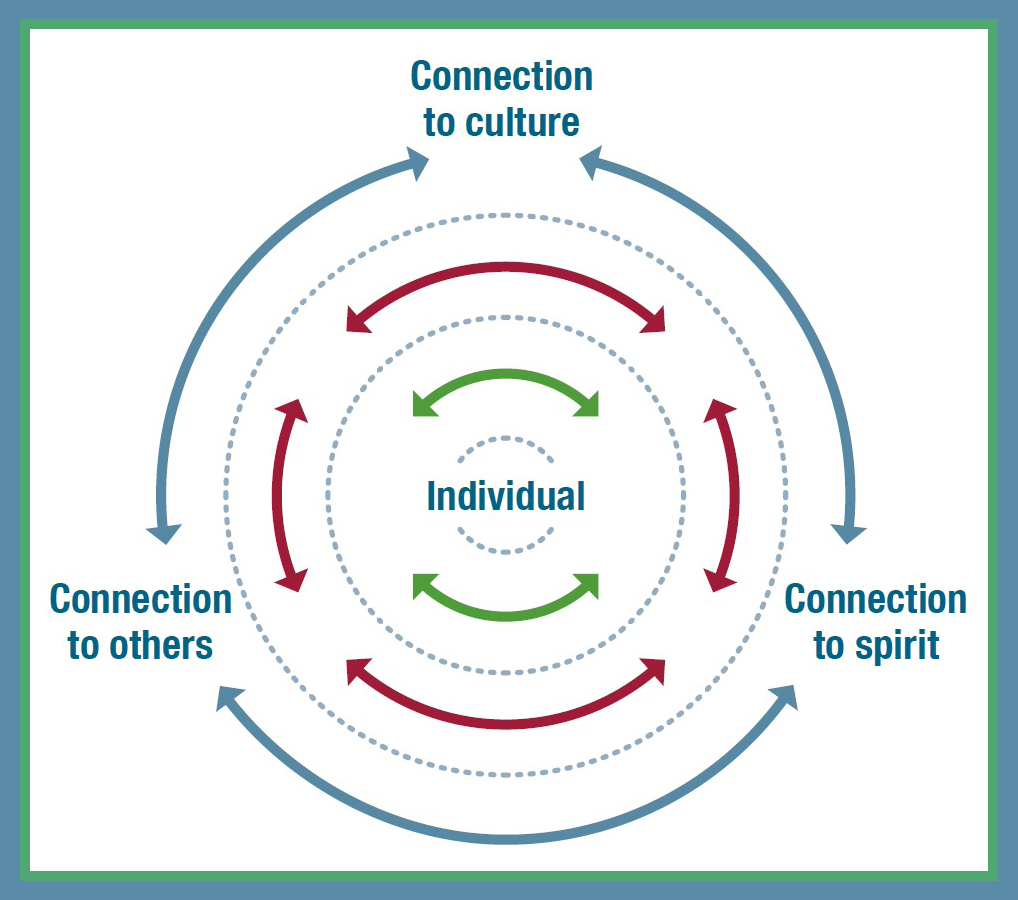
Care of patients with OUD is not linear or one size fits all. Options to engage in recovery services should be flexible and community focused.
- Focus on treatment successes rather than problems.
- Help communities build positive connections with events that do not center around opioid/substance use.
Effective OUD treatment and recovery begin with creating non-judgmental care spaces, ensuring access to medications across settings, connecting patients to support systems, and promoting harm reduction strategies at all stages of care. The IHS developed evidence-based resources to support prescribers and health systems in expanding access to MOUD and facilitating seamless care coordination.
Identifying and addressing OUD: high-level overview of key messages including stigma, screening, diagnosis, and initiating treatment [PDF - 1.6 MB]
Treating OUD and supporting recovery: more in-depth clinical information on these key messages [PDF - 245 KB]
Management of opioid use disorder across the care continuum [PDF - 6.1 MB] (*follow the instructions on page 47 to claim continuing education credit)
Q&A about opioid use disorder:address common myths – community audience [PDF - 154 KB]
Learning about OUD: patient brochure and overview [PDF - 1.5 MB]
Ref Card: key messages, diagnostic support, and routine care descriptions that are sometimes omitted in primary care [PDF - 244 KB]
NOTICE
Use of the information on this site is at the user's risk, and information is provided on an "as is" basis. There is no warranty or guarantee for the information provided on this site.
Drug and Alcohol Screening
IHS is expanding education and outreach that utilizes evidence-based approaches to substance use disorder care which includes enhanced universal screening and care-coordination efforts that support patient engagement and reduce opioid overdose rates.
Watch How to Use SBIRT: Identifying Those With and at Risk of Substance Use Disorder.
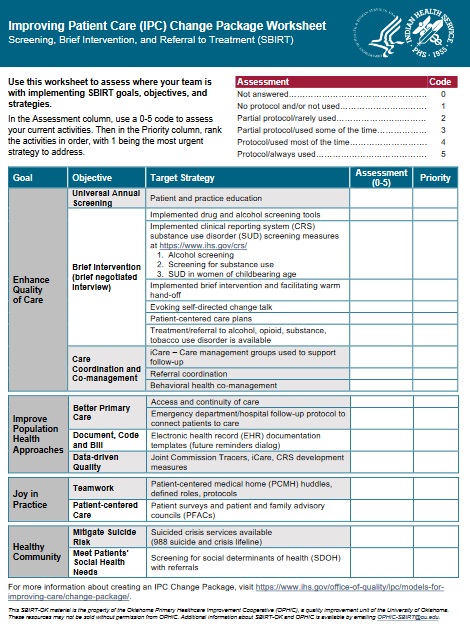
Complete the Improving Patient Care Change Package Worksheet: SBIRT Practice Assessment Tool [PDF - 191 KB] to assess where your team is in implementing SBIRT goals, objectives, and strategies.
Access the latest IHS Pain and Opioid Use Disorder Webinar recording via Zoom: Overview of New TAPS and CAGE-AID Screening Tools for Substance Use to discover insights on enhancing substance use screening.
Resource: How to Document Drug and Alcohol Screening and Assessment Tools in the IHS RPMS EHR. [PDF - 797 KB]
Trauma Informed Care

Many American Indian/Alaska Native (AI/AN) communities experience, cope with, and attempt to recover from the effects of trauma. Data shows that AI/AN people in the United States are at greater risk compared to other groups of experiencing physical, psychological, cultural and emotional traumas that may result in negative health outcomes. Causes of trauma include individual experiences of violence, personal losses (suicide, accidents, unintentional overdoses and substance use) and ongoing experiences with poverty and discrimination, in addition to health disparities.
Many AI/AN people also cope with past traumas, including historical losses of land, culture, language and people. Though these traumatic events occurred years or even decades ago, they impact the current functioning and well-being of people and their families. These cross-generational effects are known as historical trauma. Often, AI/AN people experience both personal and historical trauma.
Trauma Informed Care, a system-wide framework, facilitates recovery by creating better understanding, recognition and response to the effects of trauma. It emphasizes a holistic approach that encompasses physical, psychological, cultural, and emotional safety for everyone, including patients, staff, providers, and communities. By using trauma informed approaches, providers can offer resources, support and healing for those who suffer.
The Indian Health Service offers training and resources on the impacts of trauma to foster a more compassionate and supportive health care community.
- IHS Trauma Informed Care page
- Conceptualizing and Measuring Historical Trauma Among American Indian People [PDF - 231 KB]
Red Lake Recovery Care Stories
Provider Video: Watch Community Healing – Best Practices
Patient Video: Sharing Our Stories - Living a Beautiful Life in Recovery . Or watch the short version of the patient video.
Recovery Rack Card
Indian Health Service has created a recovery card [PDF - 595 KB] for IHS, tribal, and urban health facilities and programs. This customizable recovery card allows for the addition of specific, community-based resources to connect people to substance use treatment and recovery services.
How to Customize Your Recovery Card
- Download the recovery card [PDF - 595 KB]
- Open in Adobe
- Click on the "Edit PDF" tool in the right pane
- Add new text above "insert resources/contact info here"
- Save your edited PDF: Name your file and click the "Save" button
- Set printer settings to "print on both sides" and "flip on the short edge" on 5x7 card stock.
- Print and share.
Provider Support

Clinical pharmacists LCDR Sherry Daker, CDR Samantha Gustafson, and CDR Teresa Grund at the Red Lake Indian Health Service Hospital.
Indian Health Service (IHS) pharmacists continue to advocate for and assume key clinical roles within facilities as it relates to Opioid Use Disorder (OUD) and Substance Use Disorder (SUD) services. With numerous states expanding the scope of practice for pharmacists and increasing utilization of Collaborative Practice Agreements (CPAs), pharmacists are well-positioned to provide effective, cost-efficient, and accessible clinical services. Pharmacists are further honing their knowledge and skills to function as clinical providers and community representatives; not only focusing on pharmacological treatment, but comprehensive, patient-centered care as a whole.
IHS is known for developing many innovative pharmacy services and IHS pharmacists have practiced in expanded clinical roles for decades. Pharmacists have been advancing their practices by completing additional training and certification programs allowing for expansion in their clinical credentialling and privileging.
Clinician-To-Clinician Substance Use Warmline
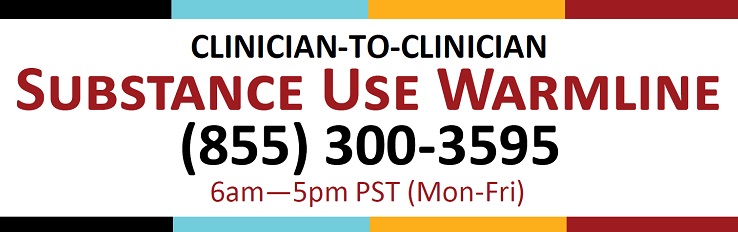
The Substance Use Warmline (1-855-300-3595) offers on-demand clinician-to-clinician support and peer-to-peer consultation from physicians, clinical pharmacists, and nurses with special expertise in substance use evaluation and management for providers managing SUDs. The warmline is available from 9am to 8pm ET (6am to 5pm PT).
IHS Pain and Opioid Use Webinar Series

The Pain and Opioid Use Disorder Webinar Series is one of many ways the IHS supports workforce development on pain management and opioid use disorder. The webinar series offers a space for healthcare providers to learn and build ideas for facility consideration. The series highlights IHS program best practices and collaborates with internal and external subject matter experts to deliver discussions on a wide array of related topics. CEU credits are available for the following professions through live webinar attendance: Medicine, Psychology, Psychiatry, Social Work, Nursing, and Pharmacy.
Previous webinar recordings (via ZOOM) are linked below:
Supporting AI/AN People Facing Serious Illness – "Pain Management Strategies in Hospice and Palliative Care" (11/6/2024)
Advancing Opioid Stewardship – "Leveraging Local Strategies to Save Lives" (8/5/2024)
TAPS and CAGE-AID Screening Tools – "Overview of New TAPS and CAGE-AID Screening Tools for Substance Use" (3/26/2024)
Treating OUD in the Hospital – "Clinical Pearls for Treating Hospitalized Patients with Opioid Use Disorder" (10/19/2023)
Cannabis and Cannabinoids II – "A Review of Cannabis and Cannabinoids: Part II" (7/23/2023)
Cannabis and Cannabinoids I – "A Review of Cannabis and Cannabinoids: Part I" (7/19/2023)
Preventing Overdose - "Preventing Overdose in Adolescents" (10/25/2022)
Do you have an idea for a webinar topic or want to share your current practices? Email Tincy Maroor, our webinar coordinator.
Family Support

Helping Babies and Supporting Parents
American Indian/Alaska Native communities have long recognized the importance of community, family, and planning for the next Seven Generations. The role of elders as cultural leaders and children as the future is well understood. Tribes understand the importance of making a positive impact on the health of communities by contributing to the well-being of mothers, babies, fathers, children, and families.
The IHS has partnered with tribes, the Office of Women's Health, the American Academy of Pediatrics (AAP), the Committee on Native American Child Health (CONACH), and the American College of Obstetricians and Gynecologists (ACOG) to develop two guidelines focused on providing standards of care surrounding screening, diagnosing, and treatment of pregnant mothers and infants affected by prenatal opioid exposure.
A comprehensive approach to care for pregnant and parenting people, infants, and children starts with prenatal care and extends well into childhood. These resources will help providers improve maternal participation in early prenatal care and promote active participation in recovery strategies to improve overall outcomes for infants born with Neonatal Opioid Withdrawal Syndrome (NOWS).
In this series of presentations, CAPT Molly Rutledge, MA, MS, Dr. Michelle Debbink, MD, PhD, Dr. Andrew Hsi, MD, MPH, and CDR Tina Pattara-Lau, MD, FACOG, share best practices, case scenarios, and program integration strategies as it relates to supporting pregnant and parenting people experiencing substance use disorders (SUDs).
AAP released clinical best practice recommendations on prevention and management of neonatal opioid withdrawal syndrome, or NOWS, for IHS,[PDF - 551 KB] tribal, and urban Indian organization health care facilities.
The recommendations are a companion guide to the clinical recommendations to improve care of American Indian and Alaska Native pregnant women and women of childbearing age with opioid use disorder.[PDF - 1.1 MB]
Some hospitals and birth centers have taken special steps to create the best possible environment for successful breastfeeding. These hospitals, called Baby-Friendly Hospitals, offer women who deliver there the information and support they need to breastfeed their infants. Learn more about the IHS Baby-Friendly Hospital Initiative.
- AAP Neonatal Opioid Withdrawal Syndrome (NOWS) Recommendation Report [PDF - 556 KB]
- American Academy of Pediatrics: Short- and Long-term Effects on the Exposed Fetus [PDF - 769 KB]
- Medicine and Pregnancy: An Overview - Centers for Disease Control and Prevention (CDC)