Opioid Stewardship in the Indian Health Service

STAY CONNECTED
Join our IHS National Committee on Heroin, Opioids and Pain Efforts (HOPE) LISTSERV to stay connected.
The Indian Health Service (IHS) Opioid Strategy supports holistic, patient-centered care that incorporates the physical, emotional and spiritual needs of each individual patient. A strong patient-provider relationship that respects American Indian/Alaska Native (AI/AN) culture and tradition through shared-decision making is an important component in developing a treatment plan. IHS aims to reduce stigma while promoting culturally-sensitive, appropriate, and effective best practices related to opioid stewardship and substance use disorders, including evidence-based treatment, recovery support, primary prevention, and other harm reduction strategies.
OPIOID STEWARDSHIP
IHS is committed to improving the way opioids are prescribed to promote patient access to safe, long-term, chronic pain and substance use disorder treatments that reduce the risk of prescription misuse, abuse, overdose, and diversion. Opioid stewardship is a key part of IHS's overall strategy to improve outcomes for patients diagnosed with chronic pain syndrome or opioid use disorder.
IHS recently released a new infographic "Advancing Opioid Stewardship: Strategies to Save Lives." The infographic outlines strategies to support robust opioid stewardship programs, offering actionable, data-driven, and patient-centric resources. Download and print your infographic [PDF - 441 KB] today!
In order to support opioid stewardship initiatives across Indian Country, IHS has released:
- A short video to provide a health-system overview of opioid stewardship as a key strategy to reduce opioid overdose mortality. Watch the overview video.
- An Opioid Stewardship Automation tool designed to assist sites and committees with evaluation of current opioid prescribing practices and facilitate discussion surrounding opportunities for improvement. The interactive tool is designed to guide team discussions as users consider core elements of opioid stewardship programs. Learn more about the Opioid Stewardship Automation tool.
- The Opioid Surveillance Dashboard (OSD) to evaluate opioid interventions and professional practice through enhanced clinical decision support tools. Data will inform system-level quality improvement strategies.
- Watch a video to learn more about how IHS is Preventing and Treating Opioid Addiction in Tribal Communities.

IHS has released a short video on the importance of opioid stewardship and strategies available to advance opioid stewardship activities across Indian Country.
Watch the Advancing Opioid Stewardship: Strategies to Save Lives video.
IHS actively coordinates, collaborates, and participates in listening sessions, formal consultations, and community roundtables to ensure agency work is aligned with the President's National Drug Control Policy Priorities [PDF - 334 KB] and relevant to tribal communities.
AI/AN populations face many socioeconomic challenges which often translate to a shortage of healthcare resources. In response, IHS is working to address Social Determinants of Health (SDoH) through a comprehensive, patient-centered, and team-based approach to patient care. The IHS supports health care practice that values health equity by striving to understand the local community and the impacts of SDoH, address implicit bias, empower the health care team and improve health literacy.
NALOXONE SAVES LIVES
On March 29, 2023, the Food and Drug Administration (FDA) approved the first over-the-counter naloxone nasal spray as an important step to increase public access to naloxone, a lifesaving medication that rapidly reverses opioid overdose. Read more about this announcement. The IHS encourages all people to get training on overdose signs and symptoms and to carry naloxone if able.
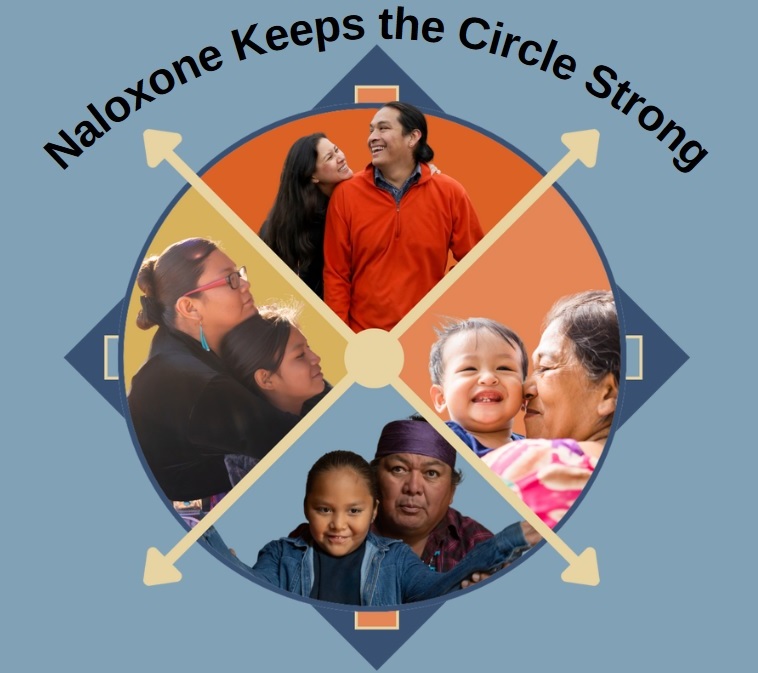
Naloxone Keeps the Circle Strong [PDF - 597 KB] and has become a standard first aid tool across the nation.
Use the Naloxone Keeps the Circle Strong Pharmacist Guide [PDF - 52 KB] as a resource to help you explain and discuss the life saving benefits of naloxone nasal spray with patients. The guide covers:
- How to introduce naloxone
- How to describe what an overdose looks like and what to do
- How to explain why naloxone is important for your patient
A naloxone in schools toolkit was released to provide an example of training plans and materials that may be used to support school implementation as the growing concern of synthetic opioids among our youth continues.
NOTICE
Appropriately prescribing opioid medications and managing chronic pain are critically important within the Indian Health Service. In May 2023, the IHS released the revised agency policy on Chronic Pain Management.
The information available on this site is intended for licensed health care professionals and adult patients. However, this site is not a substitute for clinical judgment and does not offer medical advice. Patients should consult their physicians or, in serious cases, contact emergency services. Health care professionals should confirm information available on this site with other sources.
Use of this site is at the user’s risk, and information is provided on an “as is” basis. There is no warranty or guarantee for the information provided on this site.