Monitoring
Pain experts recommend getting patients to verify treatment objectives with actual evidence, which could take the form of a letter from a physical therapist or a report from a family member. This evidence-based approach is not foolproof, but it can add considerably to the information provided by the patient. The table below offers some examples of how some functional goals can be verified.
The goal of treatment is not just to make the chronic pain patient feel better, but to help them return to their normal routine. As treatment progresses, a doctor and patient may realize that the bar has been set too high (or too low) for some functional goals. A functional goal that is too aggressive can leave a patient despairing of failure. The pain physician should know that functional goals set at the beginning of treatment can be adjusted during treatment. Many times, a patient resists achieving a goal because it hurts too much. In this case, a physician may reset the goal into incremental steps (instead of increasing pain medication). Treatment for chronic pain is a long-term process that requires adjustments.
Side effects from pain medications, usually opioids, are a constant presence. Nausea, sedation, constipation, and dry mouth are some of the effects.
| Functional Goal | Evidence |
|---|---|
| Walking | Pedometer readings or journal |
| Physical therapy | Letter from therapist |
| Employment | Pay stubs |
| Sexual relations | Report from partner |
| Social activity | Report from friend or family member |
Source: Adapted from Fishman, 2007.
Reference
Fishman, MD, Scott M. Responsible Opioid Prescribing: A Physician’s Guide. Washington, DC: Waterford Life Sciences, 2007. pp. 53–58.
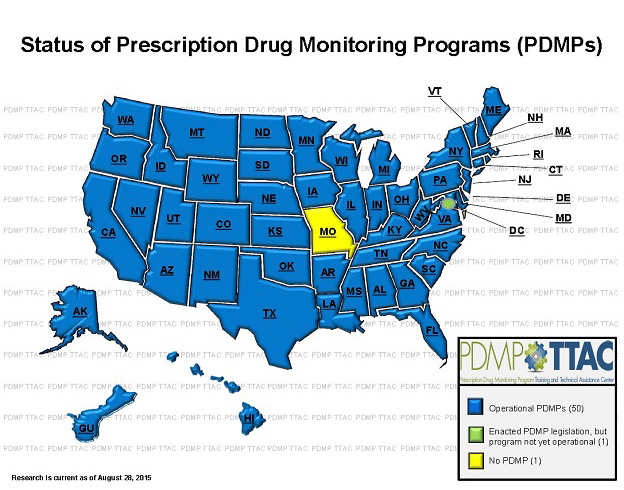
Prescription Drug Monitoring Programs (PDMPs) are a tool for prescribers and pharmacists to monitor and deter prescription medication misuse, abuse, addiction and diversion. PDMPs to date are state-run databases that collect data on controlled substances dispensed by pharmacies and prescribers operating in the state. These programs have a variety of purposes and goals, which include:
- Supporting medication safety and legitimate medical access to controlled substances
- Determining individuals who may be misusing, abusing or diverting drugs and preventing them access to controlled substances
- Assisting in the identification of individuals addicted to controlled prescription medications and intervening with treatment when necessary
- Influencing public health legislative and financial agendas by presenting prescription medication use data
- Educating the public about the purpose of PDMPs and the issues surrounding prescription drugs.
While the goals of the state PDMPs are similar, vast variations exist within state legislation, PDMP logistics, and program administration. The PDMP user should be aware of individual state licensure requirements as well as program logistics such as pharmacy frequency of reporting to fully implement PDMP in clinical practice.
Indian Health Service mandates participation with state PDMP for both prescribers and dispensers as detailed in IHS Policy.
Resources
Office of National Drug Control Policy
Prescription Drug Monitoring Program Training and Technical Assistance Center
Adherence monitoring is an integral part of treating a chronic pain patient. There are several approaches for monitoring a chronic pain patient's adherence to a drug regimen. Simply asking a patient how many pills he or she has left is a traditional, albeit imperfect, method of adherence monitoring. Random pill counts to assess overuse or diversion is a better objective measure of adherence and should be a stipulation in the controlled substance agreement. Screening tools, such as detailed questionnaires, that are usually employed at the beginning of a treatment process can be used again at some point during treatment.
Prescribing physicians can also observe behavioral and biological indicators to determine a patient’s adherence to treatment. According to Manchikanti, et al., “there is considerable research” regarding certain behaviors of chronic pain patients and whether these behaviors indicate drug misuse. The table below provides some examples.
Behaviors Predictive of Addiction
- Selling prescription drugs
- Prescription forgery
- Stealing or “borrowing” drugs from others.
- Injecting oral formulations
- Obtaining prescription drugs from nonmedical sources.
- Concurrent abuse of alcohol or illicit drugs
- Multiple dose escalation or other noncompliance with therapy despite warnings
- Multiple episodes of prescription “loss”
- Repeatedly seeking prescriptions from other clinicians or from emergency rooms without informing prescriber or after warnings to desist
- Evidence of deterioration in the ability to function at work, in the family, or socially that appears to be related to drug use
- Repeated resistance to changes in therapy despite clear evidence of adverse physical or psychological effects from the drug
Behaviors Not Predictive of Addiction
- Aggressive complaining about the need for more drugs
- Drug hoarding during periods of reduced symptoms
- Requesting specific drugs
- Acquiring similar drugs from other medical sources
- Unsanctioned dose escalation or other noncompliance with therapy on one or two occasions
- Unapproved use of the drug to treat another symptom
- Reporting psychic effects not intended by the clinician
- Resistance to a change in therapy associated with “tolerable” adverse effects with expressions of anxiety related to the return of severe symptoms
Source: Manchikanti, et al., 2008.
Checking Prescription Monitoring Programs
It is important for the prescriber to balance optimal pain control while realizing potential for diversion or opioid misuse. Prescription Drug Monitoring Programs (PDMPs) provide a useful tool to assist the clinician with determining appropriate use of controlled substance medications
Prescriber Recommendations for use of Prescription Monitoring Program Data:
- Request a PDMP report as a normal process of accepting a new patient. This information can assist the provider with determining any potential drug-drug interactions with any potential prescribed therapy.
- Prescribers should access PDMP patient data prior to appointment to facilitate meaningful interactions. Reports should be requested with every new patient encounter AND randomly for patients receiving chronic controlled substance prescriptions as part of a periodic review. Data can help prescribers to:
- Check for addiction or undertreated pain
- Check for misuse, multiple prescribers
- Check for drug interactions or other harm
- Use reports for compliance with pain agreements
- Register with state PDMP: not only for patient history reports but also for prescriber history reports. Prescriber history reports can assist you with determining fraudulent prescription activity. Self-audits should be conducted monthly.
- Use delegate accounts where authorized. Delegates can help prescribers reduce time conducting queries. Check with your state to see if delegates are allowed. Recommend a maximum two delegate accounts per prescriber. Remember that the prescriber is ultimately responsible for reports requested by the delegates.
- Document results and clinical decision making in the patient record. Check with your Area Pharmacy Consultant for your regional recommendation.
- If you detect a patient with possible aberrant behavior, it is important to take appropriate action
References
Fishman, MD, Scott M. Responsible Opioid Prescribing: A Physician’s Guide. Washington, DC: Waterford Life Sciences, 2007. pp. 58–61
Manchikanti, MD, Laxmaiah, et al. “Monitoring Opioid Adherence in Chronic Pain Patients: Tools, Techniques, and Utility.” Pain Physician 11 (2008): S155–S180.
- Move methodically; don’t rush to judgment.
- Differentiate addiction from pseudoaddiction.
- Rely on close observation, testing, and involvement of other clinicians.
Doctors who suspect their patients are violating their treatment agreements need to move methodically and not rush to judgment. Chronic pain patients can be difficult to manage; however, putting them on the defensive can have adverse effects on treatment.
A big challenge for physicians is being able to differentiate addiction from pseudoaddiction. Chronic pain patients who seek increased dosages of opioids in most cases are not addicted (loss of control, compulsion, etc.), but pseudoaddicted. Signs of pseudoaddiction include asking for drugs by name, demanding behavior, getting opioids from more than one doctor, and hoarding medications. See the table in the Adherence Monitoring section to see examples of addictive and nonaddictive behaviors. The Adherence Monitoring page also explains screening tools and drug tests that are used to maintain adherence to a treatment regimen.
A doctor who has suspicions should rely on close observation, testing, and involvement of other clinicians, such as psychiatrists or drug treatment specialists. And, relying on a written doctor-patient agreement that details the treatment process and the patient's obligations can put the patient in a less defensive mood. The Informed Consent section has a sample doctor-patient agreement.
Reference
Fishman, MD, Scott M. Responsible Opioid Prescribing: A Physician’s Guide. Washington, DC: Waterford Life Sciences, 2007. pp. 61–64.
Verifying Functional Goals
| Functional Goal | Evidence |
|---|---|
| Walking | Pedometer readings or journal |
| Physical therapy | Letter from therapist |
| Employment | Pay stubs |
| Sexual relations | Report from partner |
| Social activity | Report from friend or family member |
Source: Adapted from Fishman, 2007.
The goal of treatment is not just to make the chronic pain patient feel better, but also to restore vestiges of normal life. As treatment progresses, a doctor and patient may realize that the bar has been set too high (or too low) for some functional goals. A functional goal that is too aggressive can leave a patient despairing of failure. The pain physician should know that functional goals set at the beginning of treatment can be adjusted during treatment. Many times, a patient resists achieving a goal because it hurts too much. In this case, a physician may reset the goal into incremental steps (instead of increasing pain medication). Treatment for chronic pain is a long-term process that requires adjustments.
Side effects from pain medications, usually opioids, are a constant presence. Nausea, sedation, constipation, and dry mouth are some of the effects.
Reference
Fishman, MD, Scott M. Responsible Opioid Prescribing: A Physician’s Guide. Washington, DC: Waterford Life Sciences, 2007. pp. 53–58.