Information for Parents and Families
Pregnancy and Parental Health
Stepping into any new role may be overwhelming, especially when that role is becoming a parent. Becoming a parent may bring excitement and happiness to your life, but it also may bring new responsibility, worry, fatigue, and stress. These stressors may affect a person who is doing their best to fulfill their role as a parent, which has the potential to lead to anxiety, depression, and substance use (including alcohol, tobacco, and prescription and illicit drugs). If you have used substances in the past you may be at a higher risk of using again. Help is available for those who are dealing with substance use problems. Using illicit substances during pregnancy can cause dependence not only to the mother but also the baby.
Pregnancy and Parenting Safe Care for Substance Use Disorders

Learn about substance use, pregnancy, and caring for your mind, body, and spirit. The Plans of Safe Care Toolkit contains handouts designed to help support you and your loved ones transition into and remain in active recovery, and assist affected partners and families in growing stronger. Download and share the handouts below.
Culture Helps Us Heal
Cultural teachings are very powerful and can teach us how to be well. Growing our connection to our culture has helped many of us understand how to live well for generations. Download Culture Helps us Heal [PDF - 1.2 MB]
Getting Help for Substance Use During Pregnancy
Pregnancy is a sacred time when we make plans to care for ourselves and our baby. Pregnant women - like anyone else - can and do recover from substance use. Learn the steps toward recovery. Download Getting Help for Substance Use During Pregnancy [PDF - 1.4 MB]
Getting Help for Substance Use – For New Parents
Many people who use drugs see their infants and dream of quitting. New parents can and do recover from substance use. Learn the steps toward recovery. Download Getting Help for Substance Use – For New Parents [PDF - 1.7 MB]
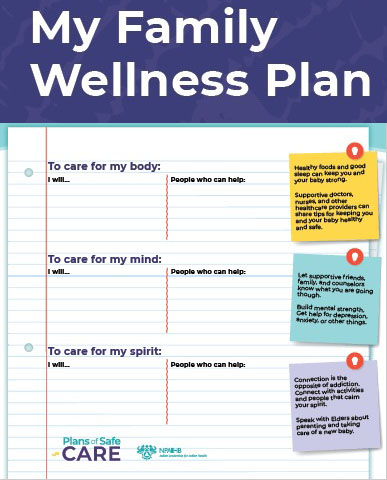
My Family Wellness Plan
Pregnancy and parenthood are sacred times when we make plans to care for ourselves and our baby. When we use alcohol or drugs, it is especially helpful to create a family wellness plan. Start your Family Wellness Plan now. Download the Family Wellness Plan [PDF - 784 KB]
Supporting Someone with a Substance Use Disorder
Know a parent or mother who uses drugs? Sometimes support can be lifesaving. Learn how you can be a good relative in Supporting Someone with a Substance Use Disorder. Download the Supporting Someone with a Substance Use Disorder [PDF - 1.7 MB]
The Truth About Substance Use and Pregnancy
To learn the truth about drug use and pregnancy, check out this handout. Download the The Truth About Substance Use and Pregnancy [PDF - 1 MB]
National Maternal Mental Health Hotline
Are you a new parent and feeling sad, worried, overwhelmed, or concerned that you aren’t good enough? You aren’t alone. You aren’t to blame. With help, you can feel better. Call or text 1- 833-9-HELP4MOMS (1-833-943-5746) to connect with counselors at the National Maternal Mental Health Hotline .
The National Maternal Mental Health Hotline provides 24/7, free, confidential support, resources, and referrals to those who are pregnant or postpartum and their loved ones who are facing mental health challenges. The service is available via phone and text in English or Spanish.
Culture and Treatment
An example of a whole-person treatment approach is the Lakota Worldview Healing for individuals and families, a powerful journey that can be a lifelong process, unique for each person and/or family. Two videos featuring Lakota members describe the what the journey is like when smooth and free from interruption, and what happens when imbalance and disruptions happen in each of the four stages of life from childhood through returning to the spirit world.
FAQs
A: Buprenorphine, or Subutex, is a common medication that can be taken for opioid use disorders to heroin and other narcotic painkillers during pregnancy. Buprenorphine has been proven to improve the likelihood of achieving sobriety from opiates while pregnant. It helps to avoid withdrawal while curbing cravings for use of other opioid drugs and allows pregnant women to focus on treatment and long-term recovery. Buprenorphine may be taken as a tablet or film (placed under the tongue or in the cheek).
A: When taken as prescribed, buprenorphine does not seem to increase the chance for pregnancy problems. Buprenorphine in pregnancy has shown to reduce drug use, improve infant birth weight, and outcomes associated with Neonatal Opioid Withdrawal Syndrome (NOWS). NOWS, also referred to as Neonatal Abstinence Syndrome (NAS), is a collection of symptoms caused by withdrawal from opioids.
A: Side effects are often rare, but babies born to mothers who used buprenorphine while pregnant may still experience NOWS, although often to a lesser extent than mother’s who used illicit drugs in their pregnancy.
A: Yes. The amount of buprenorphine in breast milk is expected to be too low to pose a problem for the nursing baby.
A: Different medical providers prescribe buprenorphine to treat opioid use disorder. All providers who prescribe buprenorphine products must have special training, and they can only take on a certain number of patients at a time. Check with your primary care doctor and see if they’re able to prescribe buprenorphine, or willing to get a waiver to prescribe it. If your primary care doctor will not personally prescribe buprenorphine, they may know another doctor who will be able to help.
Medical checkups help keep you and your baby healthy during pregnancy. This is called prenatal care. Early and regular prenatal care appointments are important when you are pregnant, especially for those with substance use disorder. Prenatal care can offer information about important steps they can take to ensure a healthy pregnancy that protects their infant.
Other Information
During pregnancy, the baby shares the medicines, drugs, nicotine, alcohol, herbal remedies, and other substances you use while pregnant. When pregnant women use street drugs (also called illegal or illicit drugs) such as heroin, methamphetamine, cocaine, marijuana during pregnancy, the baby is exposed to the drug and their effects. Opioid use disorder, opioid dependence, and poly-substance (multiple drug) use during pregnancy are medical conditions that can severely impact the health of the mother and the baby. Help is available for those who are dealing with substance use problems and their families to achieve long-term recovery.
If you have used heroin or the prescription drugs called opioids, don’t stop taking them without getting treatment from your doctor first. Abruptly stopping can cause problems for your baby. Because stopping use can cause early labor, distress to the baby, and miscarriage, those who have been using opioids during their pregnancy should not suddenly quit.
The best treatment for opioid use disorder during pregnancy includes opioid replacement medication, behavioral therapy, and counseling. Medications that are safe in pregnancy such as buprenorphine (Subutex) or methadone, when given to those who are pregnant can help them maintain sobriety and reduce complications during and after pregnancy. These drugs can help gradually reduce dependence on opioids and heroin in a way that is safe for the mother and the baby.

Neonatal Opioid Withdrawal Syndrome (NOWS) are symptoms of withdrawal that babies may sometimes develop after birth. Symptoms include:
- Fussiness
- High-pitched cry
- Difficulty feeding
- Jitteriness
- Stiff arms, legs, and back
- Difficulty sleeping
- Throwing up
- Sneezing
- Diarrhea
- Seizures
Not every baby will have all these symptoms. It depends on what drugs were used, how long and how often they were used, and how recently the drug was taken before the baby’s birth. It is important that you let your doctor know about any drugs used during your pregnancy to help deliver the best care to you and your baby.
Some babies who experience NOWS may need small amounts of a medicine while in the hospital. The goal for treating your baby is to decrease your baby’s symptoms so that they can grow and develop normally and go home as soon as safely possible after birth. While you are in the hospital, being a part of your baby’s care is important. Being near your baby as much as possible will help you get to know your baby and will also be comforting to your baby.
Ways to comfort a baby who is experiencing withdrawal symptoms include:
- Keep lights and sound low
- Hold baby skin to skin
- Use gentle touch
- Speak softly
- Swaddle your baby
- Gentle, slow rocking in an upright position
- Cradle board or Indian Swing
- Breastfeeding (if not currently using illegal substances)
- Allow more time for feedings if needed
Once your baby is home, symptoms may continue for several weeks and will gradually decrease over time. Continue to monitor your baby, and contact your doctor if:
- Withdrawal symptoms are getting worse
- Baby is not eating
- Baby is having diarrhea or vomiting
- Baby is unable to be consoled
If your baby has a seizure, stops breathing, or turns blue - Call 911 immediately for emergency help.
It’s important for you and your baby to have close follow up care with your doctor for continued health and recovery. Learn more about NOWS [PDF - 1.7 MB], recovering after birth , and caring for your newborn .
A comprehensive approach to the care of pregnant and parenting people, infants, and children affected by opioid use disorder starts with prenatal care and extends well into childhood. Comprehensive care for children’s health and wellness includes:
- Appropriate newborn care with early skin-to-skin opportunities for parent and infant
- Initiation of breastfeeding and ongoing lactation support, when appropriate
- Close observation of the newborn for signs of withdrawal
- Appropriate support and supplies that ease transition home
- Access to birth control and reproductive health care
- Appropriate treatment from supportive to pharmacologic until discharge of infant
- Established well childcare, child development, substance use disorder treatment, and well adult care through the child’s 8th birthday
The role of home visitation services is also critical to establishing wrap-around care models. Involvement of home visitation programs in community response creates an opportunity to revitalize traditional cultural practices that support children and families across all treatment and service providers.
A responsive, caring environment in the home can help reduce the impact of substance use during pregnancy. Supporting the caregiver-child attachment is critical as the family transitions to home. Early childhood development and culturally adapted home visitation programs have shown to improve long-term outcomes in substance exposed infants.
Occupational therapy may also support this transition by assisting the parent(s) and family with creating daily routines, identifying triggers, as well as stimulating opportunities to promote attachment to the newborn.
Resources
- Early Child Development - Administration for Children and Families
- Buprenorphine Fact Sheet [PDF -240 KB] - MotherToBaby.org
- NOWS Brochure Template [PDF - 1.7 MB] - Red Lake IHS Hospital
Children are often considered the most important resource in American Indian/Alaska Native communities. They will carry forward beliefs, culture and traditions to future generations. Health is influenced not only by our individual choices, but also by the circumstances in which we are born, grow up, live, work, and play. They include factors such as:
- Access to health care
- Education
- Physical and social environments
- Employment
Traditionally in American Indian/Alaska Native culture the care and education of children is a responsibility shared not just by parents, but by the extended family and the entire community. Extended families and strong connections to community can offer parenting support and link the generations together from young children to elders.
Resources
- Essentials for Parenting Teens - CDC
- Early Head Start
- Family Spirit
- Maternal, Infant, and Early Childhood Home Visiting Program (MIECHV)
- Native American Professional Parent Resources (NAPPR)
- NICWA Positive Indian Parenting
- Resources for Families - The National Indian Child Welfare Association (NICWA)
Routine visits with a primary care provider or pediatrician can help to improve outcomes for substance exposed infants. Well-child visits ensure that scheduled immunizations are given on time to prevent illness, track growth and development and address any identified concerns early, provide a chance for the parent or caregiver to ask questions, and introduce you to the care-team that can help promote wellness for the child and support families in providing care.
The recommended schedule for well child visits through age four is:
- the first week visit (3 to 5 days old)
- 1 month old
- 2 months old
- 4 months old
- 6 months old
- 9 months old
- 12 months old
- 15 months old
- 18 months old
- 2 years old (24 months)
- 2 ½ years old (30 months)
- 3 years old
- 4 years old
Babies do best on their own mother’s milk as it is nature's perfect baby food. Breastfeeding nourishes a baby’s mind, body, and spirit. There are many benefits to breastfeeding including providing ideal nutrition, protection against illness, and a healthy weight.
In some American Indian and Alaska Native communities, it is traditional for women to be secluded with their babies for several weeks after birth. Staying close to and breastfeeding your baby from the start encourages you and your baby to learn together. Breastfeeding not only provides health benefits but also increases bonding with your baby, skin-to-skin contact, and relaxation.
Women with opioid use disorder who use buprenorphine (e.g. Suboxone, Subutex) or methadone as part of a substance use disorder treatment program can breastfeed their infants. Suddenly stopping breastfeeding while taking medications for substance use disorder treatment is not recommended without first talking to your doctor. While problems are not expected, contact your doctor immediately if your nursing infant shows signs of
- Increased sleepiness (more than usual)
- Difficulty breastfeeding
- Breathing difficulties
- Limpness
If a woman relapses or uses opioids (heroin or opioid pain medications not prescribed by a doctor) she should not breastfeed until she is no longer using and has talked with her healthcare provider. When mothers use street drugs, like heroin, methamphetamine, cocaine, and marijuana they pass into your breast milk and are harmful to your baby's health.
It is important to talk to your healthcare provider to make sure any medicine (prescription or over-the-counter medication, vitamin, herbal or dietary supplement), alcohol, tobacco, and/or illicit substance you take is safe for your baby during breastfeeding. Tell each provider about any medicine you take, and don’t start or stop taking any medicine during breastfeeding without talking to your providers first.
Resources:
- American Academy of Pediatrics
- Breastfeeding Your Baby Frequently Asked Questions
- Breastfeeding - Office on Women's Health
- Breastfeeding Guide [PDF - 16.6 MB] - Office on Women's Health
- Buprenorphine Exposure fact sheet [PDF - 240 KB] - MothertoBaby.org
- Easy Guide to Breastfeeding for American Indian and Alaska Native Families
- WIC Breastfeeding Support
- WIC Native Health
- Rates of New Persistent Opioid Use After Vaginal or Cesarean Birth Among US Women - JAMA Network
Baby-Friendly Hospitals
Some hospitals and birth centers have taken special steps to create the best possible environment for successful breastfeeding. They are called Baby-Friendly Hospitals . Women who deliver in baby-friendly hospitals get the information and support they need to breastfeed their infants. Learn more about the IHS Baby-Friendly Hospital Initiative.
Resources
- Buprenorphine Locator
- Medicine and Pregnancy - FDA
- Office on Women’s Health - Pregnancy
- Frequently Asked Questions - Opioid Use Disorder and Pregnancy
- National Maternal Mental Health Hotline [PDF - 70 KB]
- To learn more about prenatal care, visit the Office on Women's Health
- SAMHSA’s National Helpline – 1-800-662-HELP (4357)
- Sub stance Use Recovery Brochure [PDF - 450 KB]
- Treating for Two
- For locations of providers use the IHS Find Health Care treatment locator.