Evidence Basis
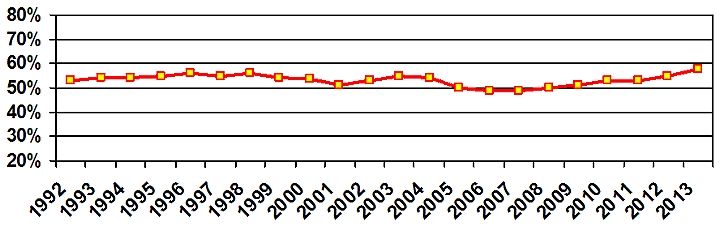
Diabetes mellitus (DM) is 2.3 times more prevalent among AI/AN's than the general US population as a whole.1 Diabetic retinopathy (DR) is a microvascular complication that develops in nearly all persons with DM and is the leading cause of new cases of blindness and visual impairment among adults.2 Timely diagnosis and treatment can very nearly eliminate severe vision loss due to DR.3 The standard of care for DR surveillance is an annual diabetic retinal examination.4,5 Only through compliance with this standard, and treatment of patients discovered to have high risk retinopathy can blindness from this disease be prevented. Historically, approximately half of AI/AN/s meet this standard of care.(Fig.1) This is costly both in terms of human suffering as well as medical economics. It is much more costly to care for the blinding complication of this disease rather than properly surveil and treat DR.6 Because of this, congress created special appropriation for use of telemedicine to increase compliance with DR surveillance standards of care in Indian Country. This technology has been deployed at 86 sites in 24 states. The following is the evidence basis supporting the use of the Joslin Vision Network at I/T/U's for the purpose of timely recognition of DR and prevention of vision loss due to this disease
ETDRS Validation – Gold Standard
The Early Treatment Diabetic Retinopathy Study defined the photographic method used to establish the legacy as well as current scientific basis for the diagnosis and treatment of DR. This method is universally accepted as the gold standard for DR surveillance, and as such is superior to a live eye examination. The Joslin Vision network was validated against this method and was shown to have substantial agreement with it. This validation study supports the JVN as equal or superior to a conventional live retinal examination for the purpose of diagnosing the level of DR and presence or absence of clinically significant diabetic macular edema (CSDME).
Sven Bursell, et al. Stereo non-mydriatic digital-video color retinal imaging compared to ETDRS 7-field 35-mm stereo color photos for determining level of diabetic retinopathy. Ophthalmology, 2001;108(3):572-585.
Clinical Validation – Community Standard
Although validation to the ETDRS provided an association with a method superior to a conventional retinal examination, a clinical validation study was conducted to provide a direct comparison to retinal examination by a retinal sub-specialist. This showed a favorable comparison between the JVN assessment of DR and that of a retinal specialist.
Anthony Cavallerano, et al. Use of JVN digital video non-mydriatic retinal imaging to assess diabetic retinopathy in a diabetic outpatient intensive treatment program. Retina, 2003; 23(2), 215-23.
Clinical Validation - Non-diabetic Pathology
Since individuals with DM are at increased risk for eye diseases other than DR, a validation study was performed to determine the ability of this telemedicine modality to detect non-DR retinal disease. This study showed excellent agreement with dilated ophthalmic examination by retinal specialists in the detection of ocular disease other than DR.
Sing-Pey Chow, et al. Comparison of nonmydriatic digital retinal imaging versus dilated ophthalmic examination for nondiabetic eye disease in persons with diabetes. Ophthalmology, 2006;108(3):833-840.
Outcome Analysis - DR Surveillance and Treatment
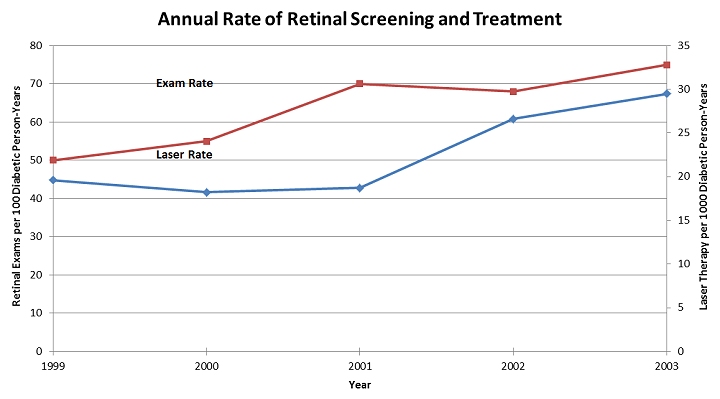
To be effective, the IHS-JVN program must have the ability to increase the diabetic retinopathy examination rate. A four year study conducted at a large IHS facility demonstrated a 50% increase in DR surveillance and a 51% increase in DR laser treatments as compared to the pre-deployment baseline year.(Fig. 2) Further review of the data showed that 100% of the increase in both measures were due to the JVN imaging activity. Ongoing review of national data shows a steady climb in the DR exam rate since the historical low in 2006-2007.(Fig.1) This is temporally related to the increasing contribution to the national rate by the IHS-JVN program.
Charlton Wilson, et al. Addition of Primary Care-Based Retinal Imaging Technology to an Existing Eye Care Professional Referral Program Increased the Rate of Surveillance and Treatment of Diabetic Retinopathy. Diabetes Care, 2004; 28(2):318-322.
Cost Effectiveness - DR Surveillance by JVN in Indian Country
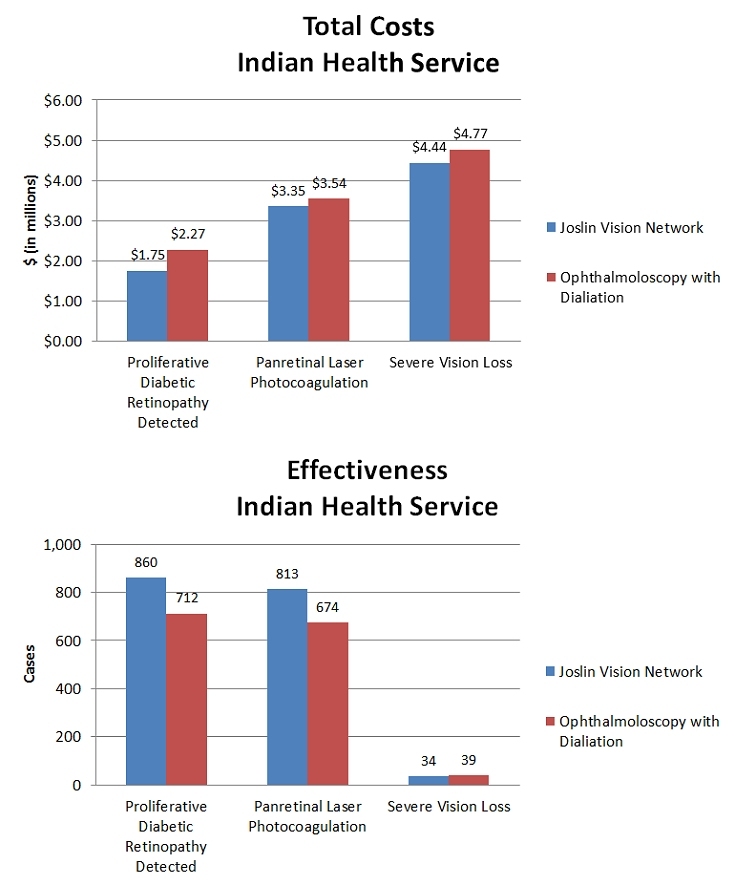
The business model for the IHS/JVN Program makes local cost effectiveness considerations effectively moot since its funding is 99% external to the hosting site. However, at the congressional appropriation level it is relevant, so a cost effectiveness study was performed using IHS specific epidemiology and costs of operations in the analysis. This study showed the IHS/JVN to be less costly and more effective than a live eye examination for detecting DR and preventing vision loss in Indian country. (Fig. 3)
Whited JD, et al. A Modeled Economic Analysis of the Joslin Vision Network as used by Three Federal Healthcare Agencies for Detecting Proliferative Diabetic Retinopathy. Telemedicine Journal and e-Health , 2005; 11(6):641-651.
References
Centers for Disease Control. National Diabetes Fact Sheet: National Estimates on Diabetes. 2011 National Diabetes Fact Sheet
Klein R, Klein BEK. Vision disorders in diabetes. In: National Diabetes Data Group, editors, Diabetes in America. 2nd ed. Washington, DC: U.S. Department of Health and Human Services, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, NIH Publication No. 95–1468; 1995: 293–336.
Early Treatment Diabetic Retinopathy Study Research Group. Early Treatment Diabetic Retinopathy Study: Reports 1-19, 1985-1995.
American Academy of Ophthalmology. Preferred Practice Patterns- Diabetic Retinopathy. 2008. Diabetic Retinopathy PPP - 2012
American College of Physicians, American Diabetes Association, American Academy of Ophthalmology. Screening guidelines for diabetic retinopathy. Ann Intern Med 1992; 116:683-685.
Javitt JC, Aiello LP. Cost-effectiveness of detecting and treating diabetic retinopathy. Ann Intern Med 1996;124:164-169.


