IHS Innovation Projects Address Social Factors in Health
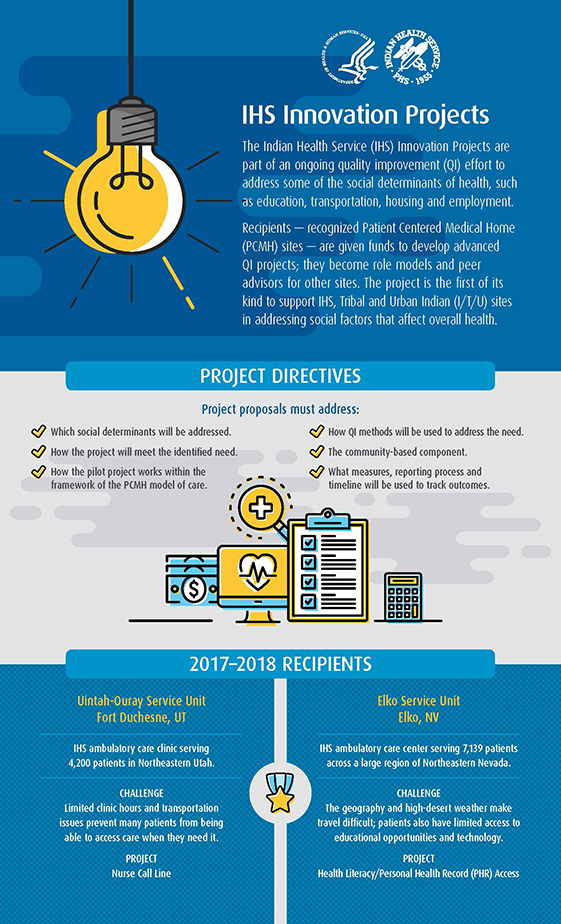
The Indian Health Service (IHS) Innovation Projects initiative is the first of its kind to support IHS, Tribal and Urban Indian (I/T/U) sites in addressing social factors that affect overall health.
Sites are given funds to develop advanced quality improvement projects addressing these social determinants. Other facilities can learn from these pioneers and become informal peer advisors to others interested in doing similar projects.
The goal of the Innovation Projects is to strengthen the link between the clinic and the community and explore how quality improvement models can address these social factors affecting health to improve overall community health.
2017-2018 Awards Given to Utah and Nevada Sites
IHS Innovation Project Awards for 2017-2018 went to two PCMH-accredited Phoenix Area sites
The Uintah-Ouray Service Unit in Fort Duchesne, UT, received an award to provide access to care through a 24-hour Nurse Call Line.
The line gives patients after-hours phone access to timely care advice and addresses transportation and economic impediments to visiting the clinic. Before the call line was created, limited clinic hours and transportation issues prevented many patients from being able to access care when they needed it.
The Elko Service Unit's Southern Bands Health Center in Elko, NV, received an award to provide technology education using an approved PCMH health literacy model to promote use of the IHS Personal Health Record (PHR), which allows patients to access their own medical records.
The Nevada geography and high-desert weather make travel challenging in the region; patients also have limited access to educational opportunities and technology.
The project provided kiosks with public-access laptops, technical support and technology education to help patients discover the benefits of using PHR, which allows them to access their health information and communicate with their care team electronically.
Learn more about the implementation of the Innovation Projects by the Uintah-Ouray Service Unit and the Elko Service Unit [PDF – 859 KB].
2018-2019 Awards Given to Urban Indian Health Program, Great Plains Area
The Gerald L. Ignace Indian Health Center Inc. in Milwaukee received a 2018-2019 IHS Innovation Projects award for a project addressing health literacy for diabetes management.
The IHS Great Plains Area received an Innovation Project award to address transportation and access to care by creating a 24-hour nurse call line. This project is a spread of the Innovation Project initiated in 2017-2018 by the Uintah-Ouray Service Unit in Fort Duchesne, UT.
For more information about IHS Innovation Projects, please contact IPC Improvement Advisor Susan Anderson.
2020-2021
The Not-Tsoo Gah-nee Indian Health Center (Ft. Hall Service Unit) - Improving the Lives of Patients with Uncontrolled Diabetes through Collaborative Practice with Continuous Glucose Monitoring and Patient Focus Groups. The project will empower patients with real-time, continuous blood glucose level information to enhance the value of telehealth visits, to give these individuals the tools they need to make significant progress in the control of their diabetes mellitus disease process. Additionally, the opportunity to participate in focus groups specifically designed to Identify unmet community needs will reveal additional ways to positively impact community diabetic outcomes.
Wellpinit Service Unit - WSU Telehealth Collaboration with BIA Corrections/Jail on Spokane Indian Reservation. Implementation of collaborative Telehealth Services between the WSU and the BIA jail on the Spokane Indian Reservation to greatly reduce CO staffing burden, improve preventive access to care, while maintaining patient dignity. The project will promote equitable distribution of high quality health care to a vulnerable population that rarely seeks preventive healthcare, increase WSU capabilities to provide access to care through Telehealth services, develop a reproducible healthcare model for other IHS/Tribal sites to adapt to respective BIA/Tribal Corrections facilities and improve HIV testing, Hepatitis C screening, and influenza vaccine rates.
Oklahoma City Indian Urban Clinic - Redesign Facilitating, scheduling & providing Women Health prenatal services. The project will expand the OKCIC's capacity for women's health services with addition of a more comprehensive staff to address the complex health care needs of the patient population. OKCIC will hire one full-time Women's Health Nurse Navigator and one Community Health Worker (MNLPN).
The goals are to decrease wait times between appointment scheduling and reduce referrals to emergency departments and hospitalization. The long-term goal is to reduce maternal and infant morbidity and mortality in the AI/AN community. This project will likely result in a model for sparking greater systemic change towards improving the quality of care delivery and health outcomes, increased access, cost savings, improving quality and saving lives.
2021-2022
Ute Mountain Ute Health Center - Pharmacist- Led Diabetes Education and Management Clinic Integration. The project will focus on outpatient clinic integration of a pharmacist to provide increased access to and equitable distribution of quality health care. The project will provide care to high risk diabetic patients in order to decrease HgA1c in intensive management patients with baseline HgA1c>9. The pharmacist will be decentralized to the outpatient clinic for approximately 15-20 hours per week. With a dedicated pharmacist, patients can have real-time and in-depth response to diabetes medication and lifestyle questions. The pharmacist clinician can co-manage patients with their primary care providers, appointments (either phone or in-person) and can be available more often to patients, more time can be spent with them, and more issues can be addressed. This will greatly improve access to care and health equity in the Ute Mountain Ute population and surrounding areas served at UMUHC.
Whiteriver SU - Increased access and engagement to mental health care, increased percent positive PHQ2 from community that receive follow-up. The project will redesign managing the care of patients diagnosed with depression and anxiety in order to increase number of encounters where depression or anxiety POV is addressed. The project will focus on patients with existing diagnoses of depression and/or anxiety who have evidence of limited follow up with primary care or behavioral health teams, and/or who have evidence of suboptimal treatment regimens and/or medication adherence.
Western Oregon Service Unit - Addressing social determinants of health to decrease obesity rates at Chemawa Indian Health Center. The project will focus on improving the patient care experience for the population of all AI/AN patients 18 and older with a body mass index (BMI) of 30 or greater. A collaborative team of medical, case managers, integrated behavioral health, and dietitian students will be utilized to initiate an intensive team based intervention while incorporating aspects of nutritional recovery. Project will entail a redesign of clinic visits to a 90 minute nutrition specialty clinic including medical intervention, nurse case management, & behavior health counselling in order to Increase knowledge of how nutrition impacts health while decreasing BMI and weight.
Yakama Service Unit – MOVE! – The project will redesign, screen and refer patients with a BMI > 30 in order to decrease BMI in patients. The Department of Veterans Affairs has an existing program that will be adopted by the Yakama Service Unit. The program’s aim is to annually screen every Native patient who receives care at YSU for obesity, refer individuals to weight management services, and make available different treatment options that fit the needs and preferences of our patients. The project involves two changes to improve outcomes related to obesity; (1) Improve coordination within YSU (medical, pharmacy, nursing) and between the IHS-Tribal health programs (Nutrition and WIC); (2) adopt an evidence-based self-management program that focuses on health and wellness through healthy eating, physical activity, and behavior change called MOVE!.
Phoenix Area Indian Health Service- Whiteriver, Elko and Fort Yuma Service Units - Co-development of quality measures to assess the patient journey. The project will focus on co-developing a set of quality measures that will broaden the current PAIHS Clinical Quality Measure Compendium to more comprehensively assess care across the patient journey. The PAIHS will measure care delivery across all six IOM domains of quality (Safety, Effectiveness, Efficiency, Timeliness, Equity, and Patient-Centeredness). The newly developed set of measures with community representatives will reflect the patient journey, both intramurally and extramurally to broaden the targets of the interventions to include those segments of the patient journey that may currently be neglected, and often disproportionately affect underserved beneficiaries.
American Indian Health & Services (UIO) – Modernize Data Collection. The project will redesign collection and input of standard patient screening data in order to decrease time to input and document health screening information. The project will replace a manual process in the current Patient Centered Home Model with a modern, automated solution to allow patients to view, complete and sign forms electronically during a contactless digital process using tablets or their personal devices. Data can be saved directly into the Nextgen EMR in a fully reportable and searchable format. The automation will improve the number of screenings completed; increase the number of people represented in the data set; reduce time connecting patients to care managers when needs are identified and improve the experience of both patients and staff.
2022-2023
Chinle Service Unit - Improving Patient Experience of Care by Expanding Interpreter Services and Cultural Safety at Chinle Service Unit. Chinle Service Unit serves a primarily Navajo population, with 75% of patients age 70 and above stating that Navajo is their preferred language. Currently at Chinle Service Unit, Navajo interpretation services are available via a telephone interpreter service, or by utilizing the services of a single on-site Language Specialist who covers the entire service unit; high demand but not always available. No official certification for Navajo Medical Interpreting exists. The project will expand the ability to offer interpretation services and patient assistance in the Navajo language. A system will be created for developing and supporting local staff to either become interpreters themselves, or demonstrate increased ability to assist patients using their Native language. The intervention will also utilize “Interpreter Huddles” and development of a local competency for Navajo medical interpreting, or “toolkit.”
Gallup Indian Medical Center - Improving Quality of Heart Failure Care for Patients at Gallup Indian Medical Center.The project will entail implementation of a tele-mentoring quality improvement heart failure model at GIMC to improve uptake of guideline-directed medical therapy (GDMT) and study its effectiveness to increase rates of GDMT among heart failure patients. The use of CARE will identify HFrEF patients who meet clinical criteria for, but are not on appropriate therapy, and implement a model that supports primary care physicians at GIMC with cardiology tele-mentorship. The team will evaluate its effectiveness by evaluating rates of appropriate therapy pre- and post-implementation of this model.
Yakama Service Unit - Telehealth for chronic conditions. This project will address a Yakama Service Unit deficiency in patient and provider utilization of the IHS PHR, which serves as the approved secure messaging portal for asynchronous communication with patients (direct email and text messaging with patients are strictly prohibited by IHS policy). YSU has the infrastructure already established to communicate with patients through the electronic health record. A “Kiosk” will be created near patient registration to facilitate patient enrollment into PHR. Remote Patient Monitoring will be the second function of this project providing blood pressure cuffs and scales to give to patients who are being treated for high blood pressure and/or obesity. While counseling and consulting Services will be provided synchronous audio-video encounters provide an option for certain chronic condition follow-up appointments, specialist consults from an urban area, and when the nature of the encounter is primarily educational. This project will create a designated room for telehealth care by medical staff with equipment purchased through the project.