2023 Hope Newsletters
Indian Health Service National Committee on Heroin, Opioids, and Pain Efforts (Hope Committee)
Indian Health Care: Ensuring a Coordinated, Holistic Response to the Opioid And Heroin Epidemic
January 2023
The CDC released new clinical practice guidelines on opioid prescribing for pain. The guideline provides updated recommendations for the treatment of acute, subacute, and chronic pain. The new guideline broadens the scope of the clinical audience to include additional practitioners, which further supports integrated care team models. For example:
Outpatient Clinicians: Dental and other oral health clinicians, Emergency clinicians managing pain for patients being discharged from emergency departments, Surgeons, Occupational medicine physicians, Physical medicine and rehabilitation physicians, Neurologists, Obstetricians and Gynecologists, Pharmacists
Primary Care Clinicians: Family physicians, Nurse practitioners, Physician assistants, Internists
The guidelines now recommend separating initial and ongoing opioid therapy, both requiring a risk versus benefit conversation between the clinician and patient. The guideline also discusses recommendations for appropriate opioid tapering, considerations for opioids dosages and guidance on non-opioid options for pain treatment.
The heart of the new guidelines support a strong patient-provider relationship and treatment plans developed through a shared-decision making process. The IHS opioid strategy supports 3 essentials of good pain management:
- Promotes overall patient wellness through individualized care planning and patient goal-setting that incorporates patient preferences, culturally responsive practices, and local resources
- Uses patient-centered, interdisciplinary and integrated systems to deliver evidence-based treatment and care
- Establishes metrics to monitor pain care and outcomes at both the individual and population level
Opioid Stewardship
Unsure Where to Begin? Start here:
1. Look at local dispensing data and attend IHS OSD Office Hours and
2. Screen for SUD and link patients to treatment
3. Promote universal access to naloxone: visit HOPE’s naloxone page

IHS recognizes the complexity of implementing and sustaining evidence-based strategies for treatment of pain and opioid use disorder. Developing innovative approaches to the opioid crisis and sharing best practices through enhanced communications is fundamental to the overall IHS opioid strategy. Effective opioid stewardship strategies emphasize safe opioid prescribing, team-based care, leadership support, and use data to inform clinical decisions that will improve health outcomes. The IHS Opioid Surveillance Dashboard (OSD) is a tool used to support local stewardship initiatives.
- Register now for the 2023 Office Hours to ask questions, understand OSD capabilities, and provide feedback on utility
- Three videos were released to support dashboard integration into facility opioid stewardship activities: IHS OSD Overview , and Incorporating data
CDC Guideline for Prescribing Opioids: At-A-Glance Recommendations
- Non-opioid therapies are at least as effective as opioids for the treatment of many types of acute pain.
- Non-opioid therapies are preferred for the treatment of subacute and chronic pain.
- Immediate-release opioids should be prescribed for initial opioid therapy (rather than extended-release or long-acting opioids).
- If prescribing opioids, the lowest effective dosage should be initiated for opioid-naïve patients with any type of pain.
- If patients are already on opioid therapy, carefully weigh the benefits and risks of changing dosages and exercise extreme care.
- Prescribe only the quantity of opioids needed for the expected length of pain severe enough to require opioid use for patients with acute pain.
- For patients with subacute or chronic pain, evaluate the benefits and risks of opioid therapy within one to four weeks of initiating opioid therapy or escalating dosages.
- Evaluate the risk of opioid-related harms prior to initiating and periodically during continuation of opioid therapy and discuss risks with the patient.
- Review Prescription Drug Monitoring Program (PDMP) data when prescribing initial opioid therapy and periodically during continuation of therapy to assess risk of overdose.
- Consider the benefits and risks of toxicology testing to assess for prescribed medications and other controlled substances when prescribing opioids for subacute or chronic pain.
- Use particular caution and consider the risks and benefits when prescribing opioids and benzodiazepines or other central nervous system depressants concurrently.
- Offer or arrange for patients to receive treatment with evidence-based medications to treat opioid use disorder; detoxification alone is not recommended due to increased risk of resuming drug use, overdose, and death.
Summary and Review: CDC Guidelines for Prescribing Opioids
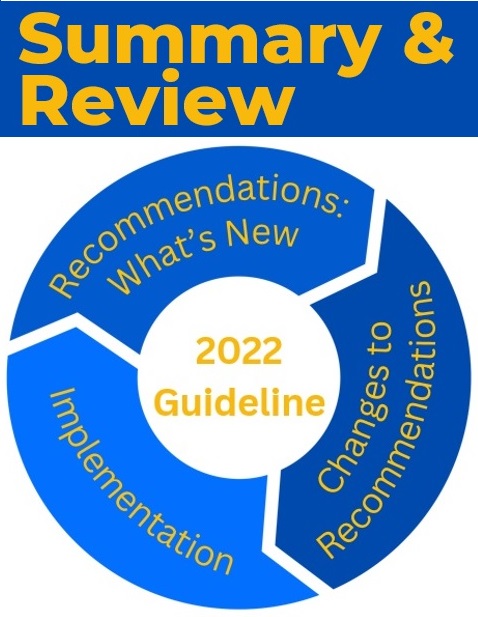
Implementation
Five Guiding Principles
- Assess and treat all pain
- Recommendations are voluntary
- Multimodal management
- Avoid misapplying guidelines
- Vigilantly attend to health inequities
Changes to Recommendations:
- Clinical Audience – broadened scope to include additional clinicians
- Initial vs Ongoing Opioid Therapy – provides separate recommendations
- Opioid Tapering – when to taper/discontinue
- Opioid Dosages – should be personalized
- Non-Opioid Therapies – consider for all patients
Recommendations: What's New
- Acute Pain – non-opioids as effective as opioids
- Subacute Pain – important follow-up periods
- Health Equity and Disparities in Pain Treatment
Newsletter written by HOPE Committee. Contact LCDR Kristin Allmaras with questions.
April 2023
Treating Substance Use Disorder: Importance of Team-Based Approaches
Integrated care teams support patient outcomes by offering comprehensive and coordinated care that is centered around the needs of the patient — known as "team-based case" where the patient is the most important member of the team. Patients and their providers create a relationship built on trust that allows for shared-decision making, co-development of treatment goals and both have an understanding of the patient's preferences related to managing their own health care.
Team-based care involves whole health approaches to health living, which is also essential to opioid stewardship. They both emphasize collaborative approaches to care and support care plans that use alternatives to opioids for pain control.
Integrated care teams can take certain actions that support team-based care and successful opioid stewardship:
- Establish adequate patient appointment time to promote positive patient relationships
- Offer the patient multiple opportunities to share their story and promote their engagement during appointments ensuring to remain in active listening mode
- Support open and friendly conversations about naloxone with any patient or family member who is curious or would benefit from the medication
- Emphasize comprehensive and culturally sensitive patient screening approaches
- If available, connect patients to community services or substance use disorder programs

Well-Balanced Opioid Stewardship Plans
Effective opioid stewardship strategies emphasize safe opioid prescribing, team-based care, leadership support, and use data to inform clinical decisions that will improve health outcomes for patients diagnosed with chronic pain syndrome or opioid use disorder(OUD).
The IHS Opioid Surveillance Dashboard (OSD) is a tool to be used to support stewardship initiatives at your site and the guidance documents can help streamline utilization of the dashboard.
IHS OSD Training Videos
- IHS Opioid Surveillance Dashboard Overview - YouTube
- Incorporating data into Opioid Stewardship Plans - YouTube
Special Populations: Pregnant Persons

Clinicians can impact and improve outcomes for AI / AN pregnant and parenting people experiencing substance use disorder (SUD). To assist these efforts, the Northwest Portland Area Indian Health Board (NPAIHB), alongside clinicians and individuals in recovery, developed a Plans of Safe Care Toolkit.
The toolkit includes a comprehensive guide [PDF - 9.3 MB] for clinicians, handouts for pregnant and parenting people and their supports, and posts to share on social media. It is designed to help clinicians care for pregnant and parenting people and their infants impacted by SUDs, support pregnant and parenting people’s transition into and remain in active recovery, and assist affected partners and families in growing stronger.
Starting Office Based Opioid Treatment? Consider these resources:
- Provider Clinical Support
- Indian Country ECHOs
- HOPE's Webinar Series
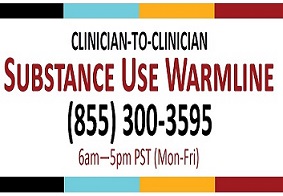
- SUD Warmline
Importance of Screening: Strategies to use in day today practice
Join the twice monthly Advancing Pharmacist Roles in Substance Use Disorder Treatment and Recovery Teams ECHO Program sessions: every 1st and 3rd Tuesday at 10 am PT/7 am ET
Knowledge is valuable to understanding a patient's health needs. When you screen for substance use, you identify patients who may have or be at risk of developing SUD. Regular and universal screening for substance use should be completed in the medical setting, regardless of medical complaint. Screening and brief intervention provides an opportunity for healthcare providers to intervene early and potentially enhance medical care by increasing awareness of the likely impact of substance use on a patient's overall health.
Consider this available training when evaluating screening strategies to employ in practice. This in-depth discussion on Screening, Brief Intervention, and Referral to Treatment (SBIRT) will illustrate best practices and practice improvement in SUD screening, examine practices for treatment referral or treatment initiation for patients screening positive for OUD, and discussion to support SBIRT implementation strategies.
Removal of the DATA Waiver: the Highlights
The Consolidated Appropriations Act of 2023 eliminated the Drug Addiction Treatment Act of 2000’s (DATA) waiver requirement for prescribing buprenorphine for OUD. The removal of administrative barriers to buprenorphine prescribing supports Indian healthcare providers in efficiently and effectively providing evidence-based treatment, strengthens the provider-patient relationship, and supports persons in recovery.
Recent Changes to the Controlled Substance Act:
- January 12: The DEA notified registrants that a DATA-Waiver will no longer be required to prescribe buprenorphine for opioid use disorder
- January 25: SAMHSA stopped accepting waiver applications and posted on their website:
"All practitioners who have a current DEA registration that includes Schedule III authoring, may now prescribe buprenorphine for OUD in their practice if permitted by applicable state law and SAMHSA encourages them to do so."
Clinical guidance available from the IHS National Pharmacy and Therapeutics Committee
- Buprenorphine/naloxone (Suboxone) is included on the IHS National Core Formulary, recommend to follow local policies and procedures related to dispensing controlled substances.
Newsletter written by HOPE Committee. Contact LCDR Kristin Allmaras with questions.
July 2023
Advancing Opioid Stewardship:Strategies to Save Lives

Opioid Stewardship (OS) is a health-system journey that involves every level of organization. OS involves a plan to ensure all the necessary steps are taken for improved processes and patient outcomes. Effective opioid stewardship strategies emphasize leadership support, team-based care, and safe opioid prescribing practices. These strategies are action-oriented, use data to inform decisions, and ensure the patient gets the support they need. There are many pieces to an opioid stewardship plan and many people involved in making sure that plan is relevant, successful and sustained.
What Can be Done? Finding Your Role
Health system leaders (Executive Leadership Team, Clinical Directors, "C-suite," Quality)
- Ensure doctors, nurses, and pharmacists have the resources they need to optimize care for patients suffering with chronic pain
- Promote access to treatment and recovery services Standardize peer review processes
- Support community engagement across the facility
All hospital and clinical staff
- Speak up! If you have an idea, share it
- Engage in workforce development activities
- Be a champion! Promote evidence-based practices
Integrated Care Teams
- Offer comprehensive and coordinated care that is patient-centered
- Build a trusted relationship through shared-decision making, co-developing goals and having a collective understanding of the patient's needs
Opioid Stewardship: Clinical Pearls and Available Resources
IHS is committed to improving the way opioids are prescribed to promote patient access to safe, long-term, chronic pain and substance use disorder treatments that reduce the risk of prescription misuse, abuse, overdose, and diversion. Opioid stewardship is a key part of IHS's overall strategy to improve outcomes for patients diagnosed with chronic pain syndrome or opioid use disorder.
To support opioid stewardship initiatives, IHS has released numerous resources, including the Opioid Surveillance Dashboard.
Opioid Stewardship Video

- Provides a health-system overview of opioid stewardship as a key strategy to reduce opioid overdose mortality
Opioid Stewardship Automation tool
- Designed to assist sites and committees with evaluation of current opioid prescribing practices
- Facilitate discussion surrounding opportunities for improvement
- Guide team discussions as users consider core elements of OS programs
Opioid Surveillance Dashboard (OSD)
- Evaluates opioid interventions and professional practice through enhanced clinical decision support tools
- Data will inform system-level quality improvement strategies
- Just getting started with the OSD? A great place to begin is reviewing site level data for co-prescribed naloxone as a key performance indicator
OSD Office Hours
- Ask questions about the dashboard and better understand capabilities
- Address real-world scenarios in dashboard use
- Teach new techniques and discuss how to optimize dashboard data
- Provide dashboard feedback, recommendations and enhancement requests
Register for OSD Office Hours
Team-Based Care
Team-based care involves whole health approaches to healthy living, which is also central to opioid stewardship. They both emphasize collaborative approaches to care and support care plans that use alternatives to opioids for pain control. Taken together, opioid stewardship is a multi-faced approach to pain management and opioid use that encompasses the whole patient – their mind and body, and their preferences, experiences, needs, and goals.
Supporting team-based care and opioid stewardship
- Establish adequate patient appointment time to promote positive patient relationships.
- Support open and friendly conversations about naloxone with any patient or family member who is curious or would benefit from a prescription.
- Emphasize comprehensive and culturally sensitive patient screening approaches.
- If available, connect patients to community services or substance use disorder programs.
Newsletter written by HOPE Committee. Contact LCDR Kristin Allmaras with questions.