Naloxone
Resources and Media
Naloxone in the Workplace Model Policy [DOCX - 215 KB]
a sample policy for responding to perceived overdose emergencies in non-healthcare, IHS office settings.
Naloxone Keeps the Circle Strong
Naloxone has become a standard first aid tool as a medication that reverses an opioid overdose. It can be given at any time, to anyone. It should be administered even if an opioid overdose is only suspected and not yet confirmed. Studies have shown that community access to naloxone can decrease overdose death rates.(Pubmed ). IHS has released a variety of resources and tools to support naloxone training in your area, please download, use and share this information broadly.
Naloxone Keeps the Circle Strong Poster/Flyer [PDF - 593 KB]
Naloxone Keeps the Circle Strong Pharmacist Guide [PDF - 52 KB]
Naloxone Training for Community Members [PPT - 8 MB]
Naloxone Training for Healthcare Personnel/First Responders [PPT - 11.4 MB]
IHS Facility Naloxone Standing Order Template [DOCx - 26 KB]
January 2024 HOPE Committee Newsletter – Harm Reduction
Naloxone Flyers
Please consider downloading and widely distributing this educational information. These documents can be used to educate patients, family members, and healthcare personnel.
- Safety Precautions: What You Need to Know about Fentanyl [PDF - 758 KB]
- Co-prescribing Naloxone [PDF - 469 KB]
- FAQs about Naloxone [PDF - 702 KB]
Please contact a naloxone mentor in your IHS Area [PDF - 114 KB] for assistance with creating a naloxone co-prescribing initiative at your site. Mentors can provide an overview of the training materials, program best practices, and offer specific technical assistance.
Naloxone in Schools
There is a growing a concern about use of synthetic opioids, such as fentanyl, among our youth. Synthetic opioids cause overdose quickly and can be mixed with other substances, such as marijuana or methamphetamine, without the user’s knowledge. This means that someone’s first use can be fatal if synthetic opioids are present. Schools in many areas have taken action to expand access to overdose prevention efforts. The toolkit below provides an example of training plans and materials that may be used to support school implementation.
Naloxone School Toolkit
- Stop Overdose: Lifesaving Naloxone – CDC
- Opioid-related Overdose Policy Guidelines and Training in the School Setting [PDF - 850 KB]
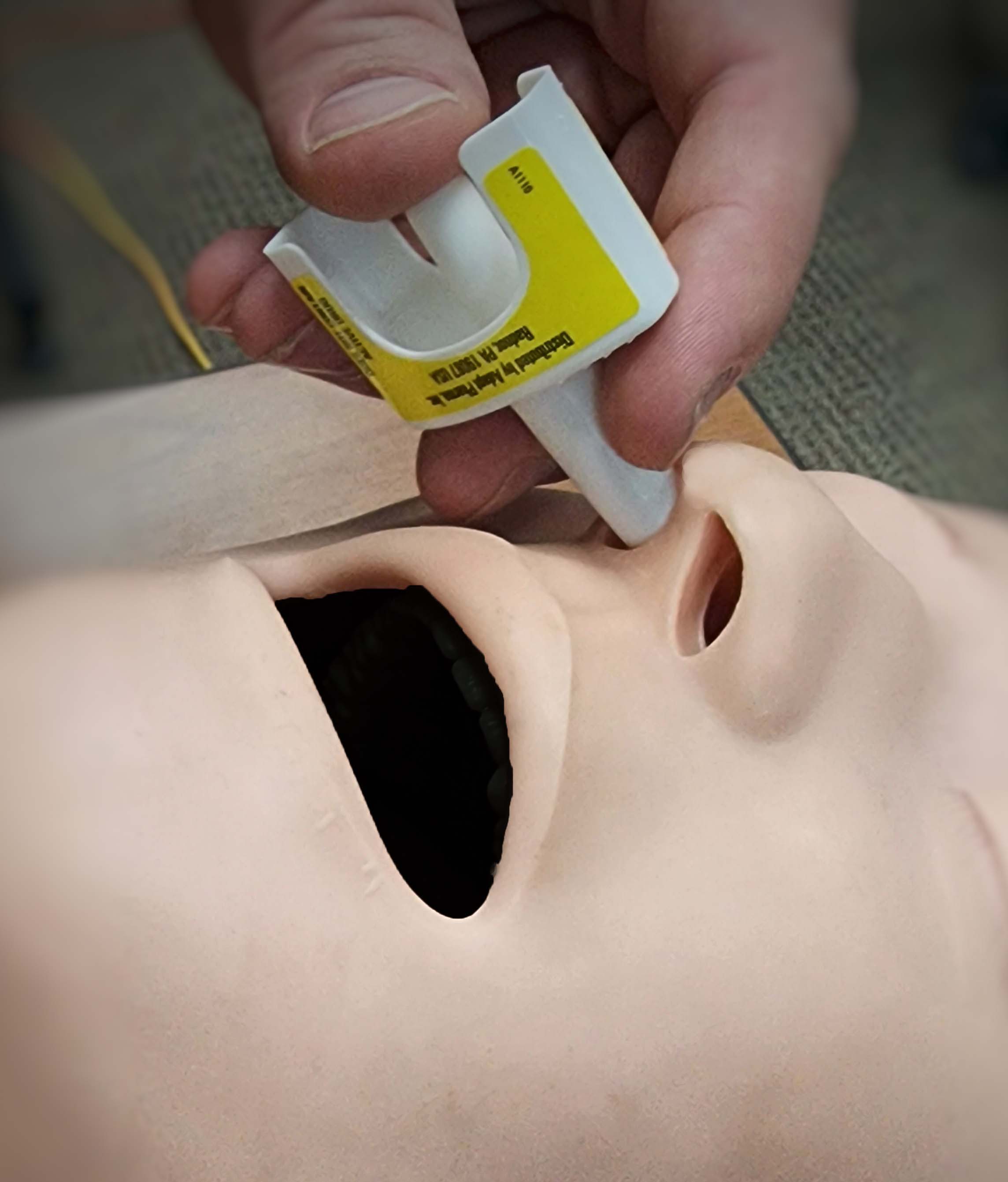
- Narcan (naloxone) Quick Start Guide [PDF - 1.3 MB]
- Naloxone School Training Questionnaire Template [DOCx - 15 KB]
- Naloxone Training Log Sample [DOCx - 22 KB]
- School District Naloxone Policy Sample [DOCx - 22 KB]
- School Training Plan Template [DOCx - 15 KB]
- Naloxone Training for School Staff and Educators Template [PPT - 1.8 MB] – see (Appendices C and D: Naloxone Skills Checklist)
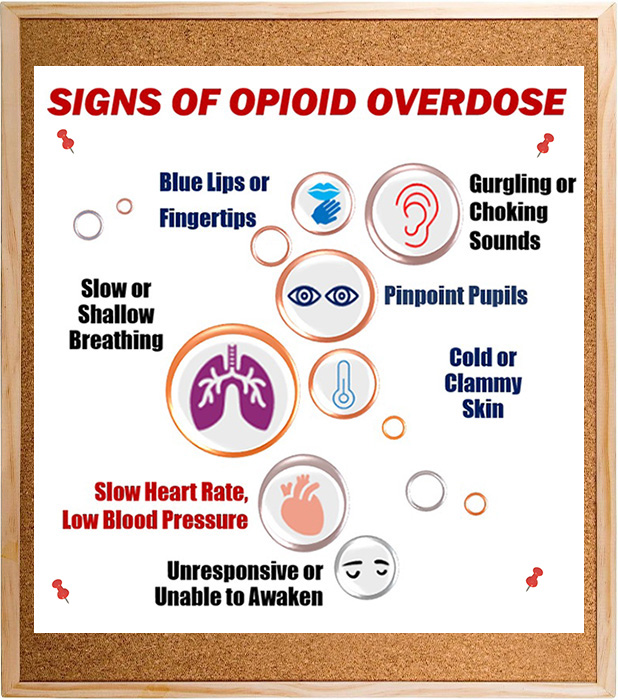
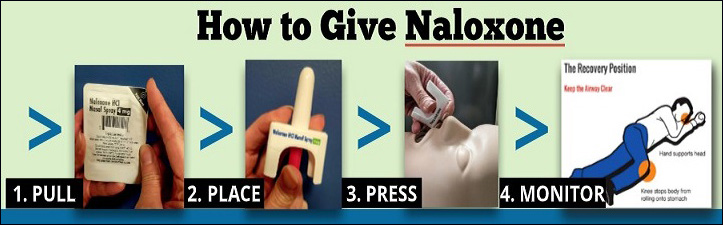
Opioid overdose can occur anywhere, at any time, and in any setting. It impacts people from infancy through adulthood, and requires a prompt response. Naloxone is a life-saving medication that rapidly reverses the effects of opioid overdose. It is quick and easy to administer, and can be given by trained first responders, healthcare professionals, and community members.
Opioid overdose occurs when the body has too many opioids on board, whether ingested, inhaled, absorbed, or injected. This amount varies for everyone, so there is no way to know how much is too much. That makes access to naloxone a vital component of harm reduction and emergency response strategies.
While opioid overdose can occur in anyone using or exposed to opioids, certain groups may be at increased risk. These include:
- Patients receiving rotating opioid medication regimens (putting them at increased risk for cross-tolerance)
- Patients discharged from emergency medical care following opioid intoxication or poisoning
- Patients with a history of substance use whom are prescribed opioids for acute care
- Patients who recently completed a detoxification program or were released from a corrections setting (i.e. reducing their opioid tolerance after an extended period of time)
Naloxone works to reverse overdose symptoms by restoring normal breathing and heart rate. It does not cause negative effects in someone whom is suffering a different type of medical emergency, and is therefore recommended to use in response efforts. Results can be seen within 2-3 minutes, but repeat doses are often needed for full reversal. Please refer to the available trainings and resources to learn more.
Opioid Overdose and Naloxone Reversal: Simple Steps to Saving Lives across Indian Country
Early access to naloxone has shown positive outcomes on reducing opioid related deaths. Healthcare professionals can reduce risk of harm by prescribing naloxone to patients that are on opioid therapy, a practice called co-prescribing, while providing patient education. Resources to support co-prescribing are shown below.
Resources
- Example Collaborative Practice Agreement [DOCX 29 KB]
- IHS Facility Naloxone Standing Order Template [DOCX 26 KB]
- Naloxone Pharmacist Guide [PDF - 52 KB] – assists pharmacists start the conversation about naloxone
Naloxone Electronic Health Record (EHR) Considerations
Consider adding naloxone to your EHR menu or include it in an order set to encourage providers to order naloxone along with an opioid prescription. For technical assistance, contact Katie Johnson or John Lester.
In 2015, IHS signed a Memorandum of Understanding (MOU) [PDF - 1.6 MB] with the BIA which allows IHS to provide BIA law enforcement officers with training and naloxone kits.
In addition, IHS, through its Area Offices, may enter into a Tribal MOU [PDF - 1.6 MB] with Tribes. The Agreement will allow for the transfer of naloxone kits from an IHS facility to Tribal First Responders, who are Tribal employees designated to immediately respond to an emergency in the tribal communities.
IHS-BIA First Responder Naloxone Training Program
- First Responder Training Program Presentation [PDF - 2.3 MB]
- First Responder Training Manual [PDF - 2.1 MB]
IHS-BIA First Responder Program Forms
- Standing Order [PDF - 796 KB]
- Acquisition Form [PDF - 860 KB]
- Naloxone Deployment Reporting Form [PDF - 859 KB]
IHS-BIA Naloxone Training Forms
- Pre- and Post-Training Questionnaires [PDF - 84 KB]
- Naloxone Competency Quiz [PDF - 65 KB]
- Naloxone Competency Quiz – Answer Key [PDF - 80 KB]
- Competency Checklist: Narcan® nasal spray only [PDF - 186 KB]
- Competency Checklist: Narcan® nasal spray and Injection w/ Atomizer [PDF - 77 KB]
- Naloxone Training FAQs [PDF - 83 KB]
The Knowledge Center is a Technical Assistance (TA) hub developed by SAMHSA that provides an overview of all current TA efforts with the Substance Abuse and Mental Health Services Administration (SAMHSA) and contributing Health and Human Services (HHS) partners.
Office of Tribal Affairs and Policy (OTAP)
The OTAP serves as the agency’s primary point of contact for tribal governments, tribal organizations, and federal agencies on behavioral health issues that impact tribal communities. Learn more about SAMHSA’s support for tribal affairs and its commitment to ensuring that American Indians and Alaska Natives have access to culturally competent prevention, treatment, and recovery support services.
Office of Indian Alcohol and Substance Abuse (OIASA)
The OIASA and its federal partners provide tribes with prevention and treatment resources as required by TLOA.
SAMHSA Tribal Training and Technical Assistance Center (TTAC)
The Center offers TTA on mental and substance use disorders, suicide prevention, and mental health promotion using the Strategic Cultural Framework.
Download and customize these naloxone documents and post at your facility and throughout your community.
- Find Connection to Care Card Sheet [PPT 203 KB]
- Naloxone sign [PDF 203 KB]
Educate your community on "Good Samaritan" laws. Good Samaritan laws create immunities or other legal protections for people who call for help in the event of an overdose. Some states have passed comprehensive Good Samaritan overdose prevention laws that provide broad protection. Other states have passed laws that consider seeking medical assistance for a person experiencing an overdose as an affirmative defense, or as a mitigating factor during sentencing.