2022 Hope Newsletters
Indian Health Service National Committee on Heroin, Opioids, and Pain Efforts (Hope Committee)
Indian Health Care: Ensuring a Coordinated, Holistic Response to the Opioid And Heroin Epidemic
January 2022
In this issue: Newly Released Recovery Rack Card, Substance Use Warmline, Virtual Naloxone Training, and Pharmacist Echo Sessions

Indian Health Service works to promote and provide holistic prevention, treatment, and recovery services for mental health and substance use disorders, as well as common co-occurring disease states. The IHS recognizes that each person’s pathway to recovery is unique. Medical staff honor their journey by acknowledging the different experiences and needs of each patient and creating treatment plans that are tailored to align with a patient’s culture, identity, background, and community. To assist with sharing this focused message, IHS has created a recovery card for IHS, tribal, and urban health facilities and programs.
WHAT IS IT?
A customizable recovery card to connect people to substance use treatment and recovery services.
HOW CAN I CUSTOMIZE IT?
Add specific, community-based resources to the back side of the card. For information on how to customize your recovery card, please follow the how-to-guidance.
WHY USE IT?
More than 100,000 people have died from a drug overdose in the United States during a 12-month period ending in April 2021, reaching the highest number ever recorded according to provisional data released by the Centers for Disease Control and Prevention. Social isolation and pandemic-related stress can increase susceptibility to substance misuse and relapse. Now, more than ever, it’s imperative to support access to treatment and recovery services.
Substance Use Warmline Available for IHS Providers
- Quick on-demand Clinician-to-Clinician consults
- Subject matter experts, one phone call away
WHAT IS IT?
An on-demand, free, and confidential resource for clinicians to use to seek support on patient cases and clinical interventions. Calls are welcome from all health care providers and disciplines in IHS federal, tribal, and urban facilities.
Cases can also be submitted online.
WHEN TO USE IT?
Do you need guidance? Are you short on time? Consulting on a complex case?
Ask questions and get quick answers on any substance use disorder (SUD) topic. Staff stay informed on the latest guidelines and medical literature to provide the most recent clinically supported advice.
Clinical staff can advise on all aspects of SUD management, including:
- Assessment and treatment of opioid, alcohol, and other substance use disorders
- Methods to simplify opioid-based pain regimens to reduce risk of misuse and toxicity
- Use of buprenorphine and the role of methadone maintenance
- Withdrawal management for opioids, alcohol, and other CNS depressants
- Managing substance use in special populations (pregnancy, geriatric, HIV, hepatitis)
WHAT TO EXPECT
- Call 1-855-300-3595. calls during regular hours will be screened by a specially trained advanced practice nurse after a quick caller registration process
- Detailed case information will be obtained, however, no protected health information is collected
- Case information will then be relayed to principal substance use consultants as indicated (the team includes expert Addiction Medicine certified physicians, clinical pharmacists, and nursing professionals),who will complete the consultation
- If screeners are unavailable or if contacting the Warmline after hours,voicemail capabilities and call-back information will be available.
- The process takes about 20 minutes (depending on the complexity of the case and co-morbidities)
WANT TO LEARN MORE?
Visit the provider considerations page.Check out the new Virtual, On-Demand Naloxone Train-the-Trainer Course
Pharmacist Echo
Join the twice monthly Advancing Pharmacist Roles in Substance Use Disorder Treatment and Recovery Teams ECHO Program sessions: every 1st and 3rd Tuesday at 10 am PT/7 am ET
Newsletter written by HOPE Committee. Contact LCDR Kristin Allmaras with questions.
April 2022
Provider Considerations: Expanding Access to Treatment
In April 2021, regulatory requirements were eased through updated Clinical Practice Guidelines. Qualified practitioners are now eligible to obtain an “X-waiver” to administer, dispense, and prescribe buprenorphine for the treatment of opioid use disorder (OUD) for up to 30 patients per year without the previously required training. Providers submit an application, known as a Notice of Intent , to access the exemption related to the specialized training requirements. If a qualified provider is interested in increasing patient limits (>30 patients per year), one can submit an application following the initial certification year with proof of successful training completion.
This exemption is in place in hopes of reducing administrative barriers in obtaining an X-waiver, ultimately increasing access to OUD treatment services. As some providers may be embarking on new journeys with patients diagnosed with substance use disorder, the IHS remains committed to supporting providers, patients, and families by recently adapting provider and patient treatment booklets for OUD.
The provider quick reference is an evidence-based tool to assist providers with diagnosing, treating, and prescribing medications for OUD. Additionally, the patient booklet provides patient and caregiver information about opioid use disorder, including treatment, recovery and overdose prevention. Both booklets have been adapted for the American Indian/Alaska Native population and provide culturally-sensitive considerations when treating OUD.
Federal IHS sites have received a sample shipment of these booklets which are intended to be resources for local sites and for providers to use at their discretion. For additional ordering information, please contact LCDR Kristin Allmaras or LCDR Sherry Daker.
The HOPE Committee has resources and training opportunities offered on their website and additional training is available that may be beneficial for healthcare providers and patients as they continue their journey to recovery.
- To ensure access to Medication Assisted Treatment (MAT), IHS released the Special General Memorandum 2019-01. All IHS federal facilities will identify OUD treatment resources in their local areas and create an action plan to provide or coordinate access to MAT, increasing access to culturally appropriate prevention, treatment and recovery support services.
- View or complete the online waiver notification form
- For clinical support, consider contacting the Substance Use Warmline
Harm Reduction Strategies: Fentanyl Test Strips
Harm reduction describes a positive approach to reduce the harm that may come from substance use. This can include individual or community- based safety practices aimed to improve overall health, wellness, and safety. The use of fentanyl test strips (FTS) provides an effective means of harm reduction by identifying fentanyl, an extremely potent opioid, in drug samples prior to use. This allows for overdose prevention measures to be employed should fentanyl be present.
When fentanyl is made by unregulated sources it can carry additional risk, which increases the possibility of unintentional overdose which may lead to death. It can be packaged and sold as named products, or added to other such as heroin or methamphetamine. This makes an expectedly "safe" amount of a substance extremely dangerous when buyers are unaware of its contents. Furthermore, DEA lab tests have revealed that four out of every ten pills with fentanyl contain a potentially lethal dose. Providing education on these risks can empower communities to stay safe and explore harm reduction strategies to save lives.
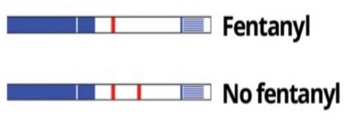
The use of FTS is quite simple, as each strip is intended for single-use when immersed in substance residue. Results are typically visible within 5 minutes, and are easy to interpret as shown in the picture below. They are inexpensive, available from a variety of suppliers, and have been used for years in many areas via syringe service programs*. Expanded access has been supported by the Biden-Harris Administration with action taken to reduce barriers to product procurement. To learn more and educate your community, please see the resources below.- Fentanyl Test Strip Education: Directions for Use and Safety Tips for Fentanyl-Containing Products
- Harm Reduction Tips
- Obtaining FTS within your facility*
*State and tribal laws regarding the consideration of FTS as drug paraphernalia may vary. Please consider the implications of these laws in your area prior to product deployment. Contributions by LT Hannah Moses and LCDR Samantha Gustafson
Accessing Naloxone
Naloxone saves lives. A virtual, On-Demand Naloxone Train-the-Trainer course is available! Learn more about the importance of naloxone products
Provider Considerations: Long-Acting Buprenorphine
Various buprenorphine formulations exist and continue to have an established role in treating OUD. Long-acting buprenorphine formulations offer patients and prescribers options to accommodate patient needs and allow further tailoring of a patient-specific treatment plan. Long-acting formulations may play an important role in OUD treatment in a select patient population such as persons at risk for non- adherence or misuse, patients with transportation issues needing supervised dosing, and patients with anticipated complicated transitions (e.g., hospital discharge or detention settings).
Providers and pharmacies need to follow a number of specific steps based on federal requirements when providing treatment with long-acting buprenorphine. Consider using these tip sheets when offering these medications in practice:
- Sublocade REMS Tip Sheet
- Long-Acting Buprenorphine Products Tip Sheet
- Visit HOPE Committee's Provider Considerations webpage for details
Subscribe to HOPE's LISTSERV today!
Additional Pain and Opioid Use Disorder ECHOs
For more information, visit the IHS Pain Management site or the Opioids home page.
July 2022
ALERT: Emerging Drug Threat: Benzimidazole Class - Nitazenes
The benzimidazole structural class of opioids were developed through pharmaceutical research in the late 1950s. These products were never approved for medical use in the United States given their extreme potency. Compared to morphine, metonitazene is about 100-fold more potent and protonitazene is about 200-fold more potent as analgesics. In comparison, according to the National Institute on Drug Abuse, fentanyl is 50 to 100 times more potent than morphine.
A Reason for Concern
In 2019, isotonitazene emerged on the illicit drug market and has been involved in numerous fatal overdose events since. Because of this, the Drug Enforcement Administration designated all of the nitazene opioids within the benzimidazole structural class a Schedule I substance to avoid imminent hazard to public safety.

Will Naloxone Still Be Effective?
For over 50 years, naloxone has been the "gold standard" for reversing opioid overdoses. The effective dose is symptom driven and with potent synthetics like fentanyl, higher naloxone doses are often required for full reversal. Case reports involving isotonitazene related overdose suggest that naloxone is effective but may require even higher doses. In 2021, the Food and Drug Administration approved an 8mg naloxone nasal spray product, brand name Kloxxado, which delivers twice the dose of standard Narcan Nasal Spray (4mg). The half-life is similar, however, higher naloxone doses may result in more severe withdrawal symptoms experienced by the patient. With the landscape of emerging potent synthetics, more research is needed on the effectiveness of overdose reversal agents, as well as considerations for naloxone alternatives.
It is important to train yourself, your family, your co-workers, and your community on the identification of an opioid overdose and administration of naloxone, the opioid overdose reversal agent.
- Read the full alert brief on nitazenes [PDF - 681 KB]
- A virtual, on-demand Naloxone Train-the-Trainer course is available!
- More information is available on HOPE's Opioids website
- For clinical support, consider contacting the Substance Use Warmline
Subscribe to HOPE's LISTSERV today!
For more information, visit the IHS Pain Management site or the Opioids home page.
Recent Release: Maternal-Infant Health and Substance Use Resources
The Indian healthcare system understands the importance of building healthy communities by contributing to the overall health and well-being of American Indian and Alaska Native pregnant and parenting people, infants, partners, and families – including those impacted by substance use disorders (SUDs). Pregnancy is often described as a window of opportunity for substance use intervention because it can be a powerful motivation for change. During pregnancy, a person's need to access maternal health services increases, providing an opportunity to strengthen patient-provider relationships which has been shown to lead to better patient health outcomes.
National Maternal Mental Health Hotline Now Available: Free, 24/7, confidential support [PDF - 70 KB] for pregnant and postpartum mothers facing mental health challenges and their loved ones.
Healthy babies begin with healthy supported pregnant and parenting people and their families. Pregnancy and parenthood are sacred times where we can engage and provide evidence-based, holistic, and culturally-responsive care. A toolkit was developed to further support this care.
Fear of stigmatization, being reported to social services, and losing custody of children are barriers to care, often resulting in delayed or avoidance of prenatal care services. Today, we know that the most effective way to help a person who is misusing substances and who may be at risk for developing a SUD is early identification and intervention. Because timely intervention leads to an increased chance of long-term recovery, it is important that healthcare providers routinely screen all persons, including pregnant persons, about use of substances.
Learning and practicing use of supportive, nonjudgmental language that treats pregnant and parenting people with compassion and respect can often be a first step in establishing trusting relationships, and creates a space to better understand patients and how to support their recovery.
Increasing access to preventative comprehensive care, empowering and educating families, and facilitating greater integration of care across health systems is the best chance of promoting the health of pregnant and parenting people, infants, partners, and families impacted by SUDs. Additional resources:
- Supporting Pregnant and Parenting People Experiencing SUD in Indigenous Communities Grand Rounds
- The NW Portland Area Indian Health Board alongside Indian health Service, Tribal and Urban Indian healthcare providers, and AI/AN individuals impacted by SUDs developed a Plans of Safe Care Toolkit
- IHS HOPE Committee's Maternal and Child Health and Wellness webpage
Contributions by LCDR Sherry Daker
IHS Pain and Addiction Care in Emergency: Pilot Project Bootcamp
An initial kick-off meeting for the IHS Pain and Addiction Care in Emergency Departments (PACED) pilot projects was hosted in mid-July. During the two-day bootcamp, participants representing seven IHS Emergency Departments (EDs) received training from the American College of Emergency Physicians (ACEP) to identify and develop new systems of care and best practices to improve addiction and pain outcomes in the ED by:
- Improving patient screening and increasing access to medications for OUD
- Improving clinical care pathways following patient overdose resuscitation
- Enhancing non-opioid pain management strategies as part of opioid stewardship within IHS EDs.
Local champions will also focus on achieving PACED Accreditation, which is intended for hospitals that seek to improve pain management and addiction care for patients in the ED and recognize the need for prompt, safe, and effective pain management and substance use disorder care for patients.
Provider / Clinician Support
- Substance Use Warmline
- Pain and SUD ECHOs
Newsletter written by HOPE Committee. Contact LCDR Kristin Allmaras with questions.
October 2022
ALERT: Emerging Drug Threat:Rainbow Fentanyl

Fentanyl is a synthetic opioid that can quickly cause overdose. It is available as a prescription, pharmaceutical-grade product or an illicitly manufactured product with potency up to 50 times greater than heroin and 100 times greater than morphine. This makes it a major contributor to the 150+ synthetic overdose deaths occurring every day. In recent months, brightly colored fentanyl tablets, powder, and blocks that look like candy or sidewalk chalk have been trending across the nation. Due to their potency, very small amounts can cause damage to the brain, and lead to overdose or overdose death.
Action can be taken to save lives through prompt recognition of overdose symptoms, and administration of the opioid reversal medication called naloxone. It is quick and easy to deliver, with trainings available across the country. The Indian Health Service identifies such trainings as a key strategy to reduce mortality from opioid use disorder, empowering providers, first responders, community members, etc. to learn about and carry naloxone. To complete training, visit an IHS pharmacy or online via the IHS Naloxone Training Toolkit.
In the event you witness an overdose or identify an alarming product, contact your local authorities for assistance. Caution should be taken to avoid touching these items, although risk of absorption through the skin is minimal. Whenever possible, await guidance from law enforcement or wear medical grade gloves.
Communities, parents, and teachers should consider educating on the dangers of rainbow fentanyl and seeking naloxone training to prevent overdose deaths in their area. If you don’t already carry naloxone, please accept this challenge to do so to save lives.
Learn More
- Read the full alert on Rainbow Fentanyl
- Fentanyl Facts
- DEA Warns of Brightly-Colored Fentanyl
- DEA Fentanyl Awareness Campaign
- Opioid Overdose Symptoms
- For clinical support when treating substance use, consider contacting the Substance Use Warmline
Patient Screening and Assessment Tools: Identifying Patients with Risky Substance Use
Knowledge is valuable to understanding a patient’s health needs. When you screen for substance use, you identify patients who may have or be at risk of developing a substance use disorder (SUD). Regular and universal screening for substance use should be completed in the medical setting, regardless of medical complaint. Screening and brief intervention provides an opportunity for healthcare providers to intervene early and potentially enhance medical care by increasing awareness of the likely impact of substance use on a patient's overall health.
Why Screen for Substance Use?
- Illicit substance use is common, harmful, and has many adverse consequences.
- Only a fraction of people who need treatment for SUDs receive it each year.
- Using screening and brief intervention can make a difference in substance use behaviors.
Before your begin screening
- Determine staffing roles, including who will administer the screening instrument; discuss results with patients; and intervene and/or refer when necessary.
- Train designated staff to conduct screening, intervention, and referral.
- Decide how screening results will be used and develop a procedure for handling positive and negative results. Note: Screening is not a full assessment; refer patients for a full assessment if a problem is indicated by the screen or through discussion with the patient.
- Apply existing office procedures to screening practices, including patient documentation, consent procedures, confidentiality and HIPAA procedures, storage of records, and patient flow.
- Increase sustainability of efforts through reimbursement. Tip: read the CMS SBIRT Services Booklet.
- Establish relationships and linkages with external providers who will accept referrals for additional assessment and/or drug treatment.
- Consider patient reading level when providing educational and support materials. Because it is often difficult to determine reading level, particularly in emergency room situations, consider using materials developed for an 8th grade reading level.
Which Screening Tool Should I Use?
Choose a universal, validated screening tool. The Screening and Assessment Tools Chart provides a comprehensive guide and links to evidence-based screening and assessment tools.
Currently, IHS RPMS EHR allows for documentation of the following drug use screening tools:
NIDA Drug Use Screening Tool : screens for Alcohol/Drugs, for use with Adults, administered by Clinicians
Drug Abuse Screen Test (DAST-10) : screens for Drugs, for use with Adult patients, administered by Clinicians
CRAFFT: screens for Alcohol/Drugs, for use with Adolescents, both Self administered and administered by Clinicians
Parents, Partner, Past, and Present (4Ps) for pregnant people
Subscribe to HOPE's LISTSERV today!
For more information, visit the IHS Pain Management site or the Opioids home page.
Contributions by LCDR Sherry Daker. Please contact LCDR Daker with questions regarding appropriate documentation of screening tools.
Newsletter written by HOPE Committee. Contact LCDR Kristin Allmaras with questions.


