The Quentin N. Burdick Memorial Health Care Facility is a 27-bed facility serving approximately 15,000 enrolled tribal members of the Turtle Mountain Band of Chippewa Indians of Belcourt, North Dakota. This rural Indian Health Service (IHS) hospital in north central North Dakota does not have a liver disease specialist nearby. Despite this and other challenges, our health care facility instituted an innovative treatment program for the hepatitis C virus (HCV).
Nationwide, certain populations have higher rates of viral hepatitis. These include baby boomers, people who inject drugs, Asian Americans and Pacific Islanders, African Americans, and American Indians and Alaska Natives (AI/AN). The AI/AN HCV-related death rate is more than double the national rate. While reducing the number of new infections and deaths related to HCV is one of the goals included the National Viral Hepatitis Action Plan , curing patients is still a challenge because of lack of access to specialists and high HCV drug treatment costs. Belcourt IHS, like many rural health networks, has a shortage of primary care and specialty health care providers.
With the support from our administration, and the primary care providers, we were eager to step up and lead the HCV response. Among other education activities, we attended a two-day immersion training on HCV, and began regular participation in telehealth sessions via Project ECHO (Extension of Community Health Outcomes).
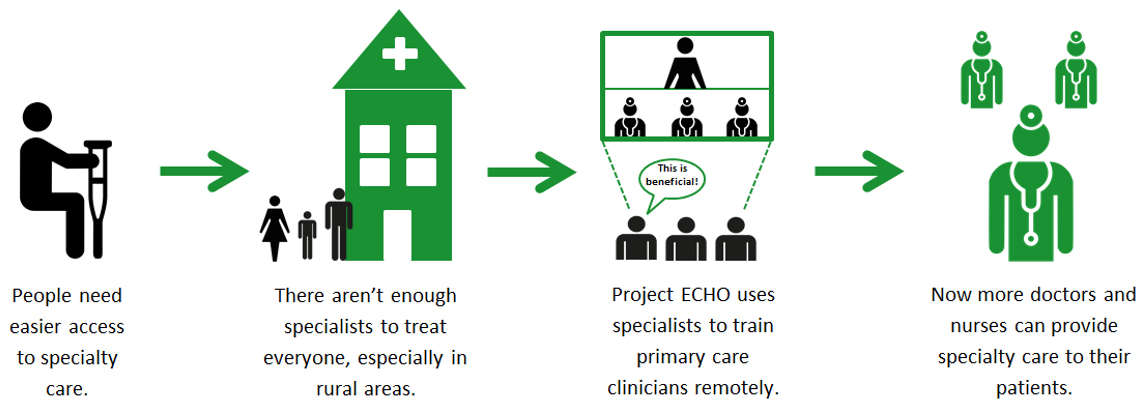
Project ECHO is a learning practice model that revolutionizes medical education and access to specialty consultation. Project ECHO exponentially increases health workforce capacity to provide best practice specialty care and reduces health disparities. The heart of the ECHO model™ is its hub-and-spoke knowledge-sharing network. Led by expert teams at the hub, videoconferencing is used to conduct virtual clinics with community providers who are often thousands of miles away. In this way, primary care doctors, nurses, and other clinicians learn to provide state-of-the-art specialty care to patients in their communities.

Once we completed the ECHO training, we began a pharmacist-managed HCV clinic at Belcourt. Following national recommendations and best practice models of care, we instituted automatic reminders that signaled clinic staff to screen patients born between 1945-1965 for HCV. Screening for HCV began increasing dramatically. In addition, we reviewed patient data to identify and follow-up with all current and past HCV patients which prioritized patients with late-stage disease for immediate treatment. This process, called empaneling, can help providers use limited resources more effectively while getting an understanding of how many patients require treatment.
Screening and empaneling patients is helpful for diagnosing and linking patients to care, but it can only assist them if treatment is available. Once HCV patients are ready for treatment, we use the ECHO model™ to confer with HCV specialists who provide guidance and mentoring, as well as assistance in development of the proposed treatment or referral plan. We then initiated treatment, with additional support from primary care providers and specialists as needed. ECHO model™ clinics for Indian Country are available nationwide to federal, tribal and urban IHS clinics. They are operated in collaboration with the University of New Mexico, as well as tribal entities such as the Cherokee Nation, and the Northwest Portland Area Indian Health Board.
From its start in May 2017, the Belcourt clinic has empaneled nearly all of its HCV patients, and rapidly linked roughly 50% of them to the HCV clinic. Of the patients who completed the pharmacist-led treatment plan, 100% are virus free and effectively cured. We have collaborated and provided trainings and support to other IHS facilities who are at various stages of developing their own primary care HCV clinic.
This HCV program, led by officers from the Commissioned Corps, is a model of collaborative practice between medical providers, pharmacists, laboratory services and case managers in the Great Plains Area.
The success of the HCV Team at Belcourt has also stimulated other sites in the area to engage in ECHO and provide HCV treatment via a Great Plains Area specific ECHO. This ECHO focuses on HCV treatment and systems issues relevant to the area and has made a targeted effort at onboarding clinics in the Dakotas, Montana, Minnesota, and other Northern Tier states. Since January 2018, 13 clinics in these states have participated in the Great Plains ECHO and 27 patients have been given recommendations for treatment. As Jessica Leston, the HCV and HIV clinical programs director with the Northwest Portland Indian Health Board recently stated to us, “the ECHO model™ has provided a process to guide transformational change for Hepatitis C treatment for patients and systems change for the clinics. That is truly making a difference and saving lives.”
Related Content:
Expanding Access to Hepatitis C Screening and Treatment in the IHS Portland Area



