Let me tell you why I’m excited, hopeful and optimistic in 2021 despite the COVID-19 pandemic. Why? It’s because of the major advances in vaccine technology over the past 30 years. Progress has been so dramatic that it is safe to say we have entered the “golden age” of vaccines. The chart below visually demonstrates this dramatic change in approach to disease treatment and prevention. Here, the number of new vaccines are steadily rising, while new antibiotics have been declining. The introduction of antibiotics peaked in the 1950s and 60s, giving way to vaccines as the preeminent infectious disease tool.
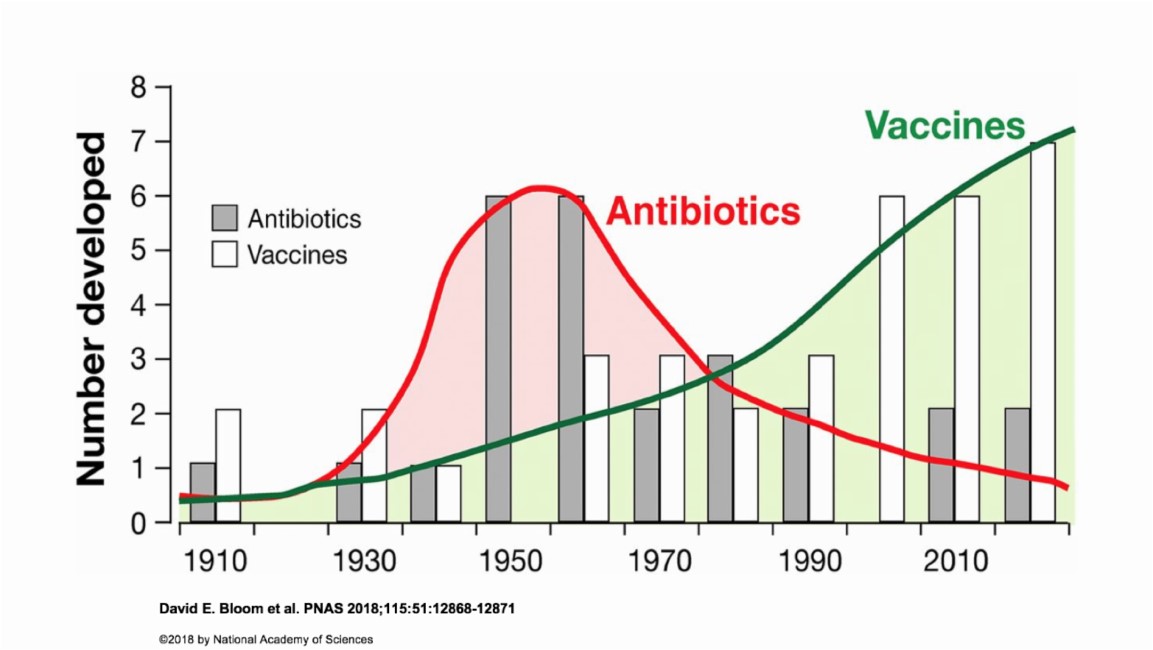
Following the triumph of penicillin, which is used to treat many different types of infection caused by bacteria, medical science succumbed to thinking that antibiotics would cure the world of infectious diseases. Amazingly and quickly, these microbial enemies mutated and developed resistance. New antibiotics were developed and then new mutations formed. Clearly, this approach was not going to lead to long term success. Wisely, a different strategy was chosen. Instead of fighting these “enemies,” we chose to leverage our amazing and elegant self-defense, using vaccinations to create stronger people with stronger, smarter immune systems.
30 years ago, when I started my pediatric medical career, the options we had for preventing illness and death caused by infectious diseases were limited to just three childhood vaccines protecting against seven diseases: diphtheria, tetanus, pertussis, measles, mumps, rubella and polio. While all children were at risk, children in Native communities, especially in Navajo, Alaska Native, and Apache communities, suffered even more. Haemophilus influenzae type b infection rates were 4 to 10 times higher than the general population, and streptococcus pneumoniae infection rates 4 to 50 times higher. Communities also suffered outbreaks and endemic disease cycles of hepatitis A, chickenpox, rotavirus, and hepatitis B infections. Over the next decade, more vaccines were developed to protect against these serious diseases.
Many parents in American Indian and Alaska Native communities had up-close and personal experiences with illness and death from infectious diseases. Their direct experience played a role in why they were more receptive to new childhood immunizations as they were introduced. As the 21st century began, with more children vaccinated from more diseases, the rates of disease fell – dramatically. As we vaccinated more children, we also saw decreased disease and death in adults. These vaccine successes built a trusting relationship that still echoes today with continued vaccine confidence.
At the same time, there were changes to the immunization ecosystem, data and programs. The 1989-1991 U.S. measles outbreak served as a catalyst, prompting the CDC and the federal government to create the Vaccines for Children program , the National Immunization Survey , and begin to leverage new computer technology to create state Immunization Information Systems. The National Immunization Survey was our nation’s first look at vaccine rates and the effectiveness of vaccine campaigns. Now, prompted by the COVID-19 pandemic, there is greater appreciation and demand for even better immunization data systems to optimize our health, which promises another leap forward.
All of these advances in vaccine development, technology, and data reporting over the past 30 years made a huge impact on our ability to fight COVID-19 today. Look back just a year ago, when all we had to offer for COVID-19 infection prevention was quarantine and social distancing. These are the same strategies that were used during the 1918 flu pandemic and even during the Black Plague in the Middle Ages! But in less than a year, we have not one, but three incredibly effective vaccines, with more in the pipeline. The previous decades of vaccine research and technology progress built the foundation that gave us the tools and ability to quickly produce these amazing vaccines.
In 2021, we have better, safer and more vaccines to strengthen people of all ages. Our vaccine advances over the past 30 years have been like going from an era of horse-buggies to jet planes. When we pause to look at how fast and how far we have come today, I believe there are plenty of reasons to be excited, hopeful and optimistic!
Increasing Routine Immunization Coverage for Pediatric and Adolescent Patients
This blog post is part of an ongoing effort to help increase routine immunization coverage for American Indian and Alaska Native pediatric and adolescent patients. A variety of resources are also available, including recorded Information Technology office hour sessions and clinically focused webinars.
To learn more about strategies, best practices, and tools to implement at the local level to improve immunization coverage rates, register here for our next webinar in the Pediatric Immunization Webinar Series on Wednesday, September 15, at 3:00 pm EDT:
Pediatric Immunizations: Best Practices and Lessons Learned
Presented by: S. Jones, BSN; D. Fuller, BSN; L. Haven, MPH; T. Tah, MBA, BSN
Related Content:
IHS Blog: Promoting Vaccine Confidence
IHS COVID-19 Vaccine Confidence Materials
CDC: How to talk about COVID-19 vaccines with friends and family



